
What 11 Billion People Mean for Disease Outbreaks

Editor's note: By the end of this century, Earth may be home to 11 billion people, the United Nations has estimated, earlier than previously expected. As part of a week-long series, LiveScience is exploring what reaching this population milestone might mean for our planet, from our ability to feed that many people to our impact on the other species that call Earth home to our efforts to land on other planets. Check back here each day for the next installment.
In mid-April 2009, samples from two California children suffering from the flu arrived at the Centers for Disease Control and Prevention in Atlanta for further investigation; something didn't seem normal about the particular flu strains they had. Local clinics and flu surveillance staff had detected a virus that had a unique genetic makeup, different from any known human flu virus. It was entirely new to science.
That was the beginning of the 2009 swine flu pandemic. Countries around the world took notice and prepared for possible outbreaks, the World Health Organization sent out guidelines to ministries of health and vaccines were developed in a matter of months. The virus, which may have started infecting people first in Mexico, spread across the globe, infecting millions of people and killing thousands before running its course, with the pandemic coming to an end in August 2010.
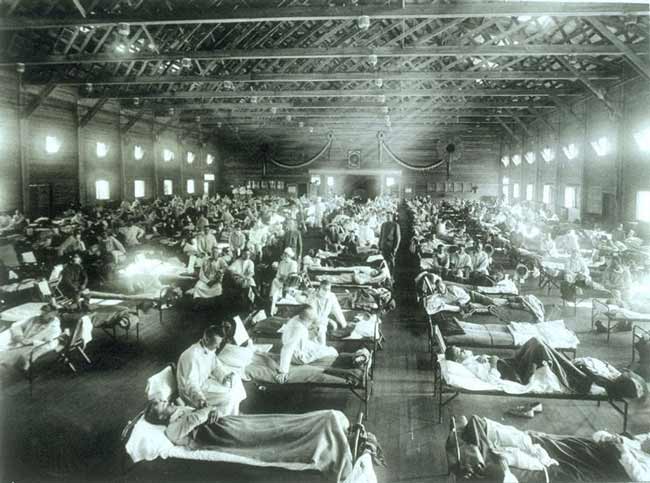
The virus was a new strain of H1N1, the influenza virus involved in the devastating 1918 Spanish flu pandemic, which killed between 30 million and 50 million people worldwide, according to the U.S. Department of Health and Human Services, more than died during World War I. The emergence of the new H1N1 in 2009 was a reminder that despite the unprecedented progress in treating infectious disease in the past decades, the looming shadow of a deadly pandemic still persists.
In fact, with every mysterious virus that surfaces, be it the 2009 swine flu, the 2002 SARS coronavirus, or most recently, MERS (Middle East Respiratory Syndrome, a viral respiratory illness that has emerged around the Arabian Peninsula and killed half of the people who have had it), the same questions come to the minds of researchers and health authorities: Is this the virus that's going to cause the next pandemic? And will humanity be able to stop it?
And now, new challenges are being added to existing ones: The latest population projections from the United Nations, announced in a new report last summer, estimate that the world's population will reach 9.6 billion people by mid-century, and 11 billion by 2100.
The sheer number of people, their interactions with animals and ecosystems, and the increase in international trade and travel are all factors that will likely change the way humanity deals with preventing and treating epidemics, experts say. In fact, the unprecedented growth of the human population in the second half of the last century — growing from 2.5 billion to 6 billion — may have already started changing how infectious diseases emerge. [What 11 Billion People Means for the Planet]
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
"There's a strong correlation between the risk of pandemic and human population density. We've done the math and we've proved it," said Dr. Peter Daszak, a disease ecologist and the president of Eco Health Alliance, who examined the link in a 2008 study published in the journal Nature.
Looking at contemporary outbreaks since the mid-20th century, Daszak and colleagues found that the rate of emergent diseases caused by pathogens new to humans has increased significantly with time, even when controlling for progress in diagnosis techniques and surveillance, which could make it only seem like diseases were on the rise. More than 300 new infectious diseases emerged between 1940 and 2004, the study found.
Some of these diseases were caused by pathogens that have hopped across species and finally into humans — for example, the West Nile virus, the SARS coronavirus and HIV. Others were caused by a new variant of a pathogen that evolved to thwart available drugs, such as drug-resistant tuberculosis and malaria.
Certain pathogens, such as the bacteria that cause Lyme disease, are not new to humans, but their incidence increased dramatically, perhaps due to changes that newly arrived humans made to the environment inhabited by animals carrying these pathogens.
In light of the continuous population growth, health authorities are calling for strengthening public health organizations, and giving more resources to systems that would protect people. Researchers are studying ways to identify viruses faster, so that vaccines could be developed early in the process, and scientists are trying to understand the complicated interactions between humans and the surrounding ecosystem, so that they could identify emerging disease hotspots and find the next emerging virus before it finds humans. All of these are done in an effort to have the new creative solutions that preventing pandemics on a populated planet would require.
"You can predict very confidently as each year moves forward, we're going to see more and more diseases emerge," Daszak said. "It's a little abstract to most people. And to be fair, it's new for scientists too."
Diseases of the future are already in nature
When Daszak and his colleagues analyzed the characteristics of emerging diseases, they found some similarities between them. All known emerging diseases were linked to sudden human population growth, new human activity in the environment and high wildlife diversity in the area where the pathogen originated.
About two-thirds of new diseases were transmitted to humans from animals, the researchers found.
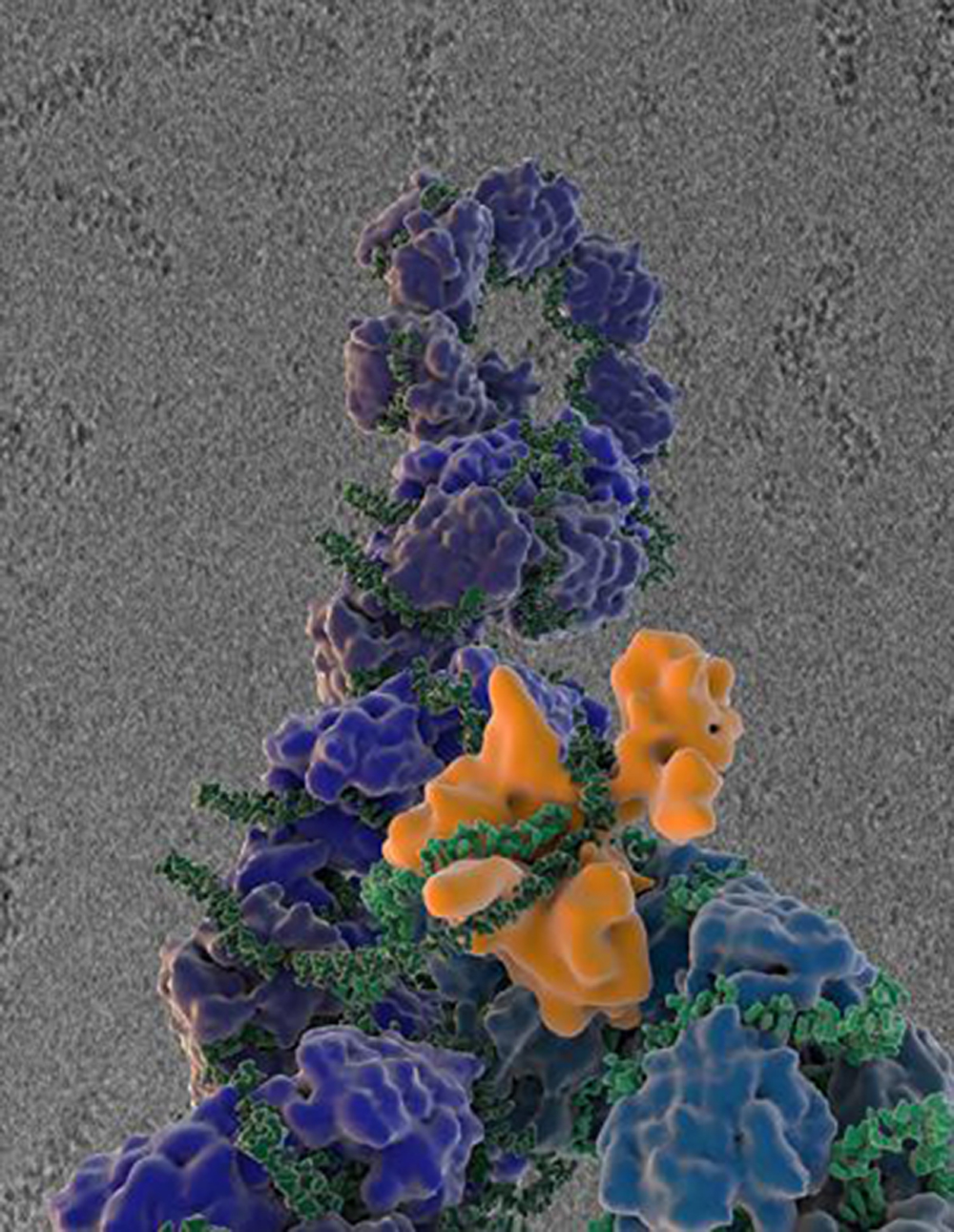
More than 70 percent of these diseases, known as zoonotic diseases, were caused by pathogens originating in wildlife — for example, the Nipah virus that causes inflammation of the brain and first surfaced in 1999 in Perak, Malaysia, or the SARS coronavirus that first infected a farmer, are both traced back to viruses in bats. [Video: Time-lapse of new infectious diseases worldwide during 1944-2004]
As humans do not often come into contact with wildlife, such pathogens should theoretically not pose much danger to people. But the pathogens can make the leap to humans by first infecting other animals that humans do come into contact with, such as domestic pigs. The animals serving as the middle link of this disease chain, however, have to be in places in some overlapping territory, which occurs when burgeoning populations push people into wild areas where humans once rarely, if ever, ventured.
"Each wildlife species carries a bunch of microbes, most of them we've never known about," Daszak said. "When you build a road into a new patch of rainforest, you put a pig farm in there, people move in and come into contact with these pathogens."
The number of pathogens originating in wildlife and infecting humans has increased with time, too, Daszak's research shows. In the last decade of the 20th century, such pathogens were responsible for more than half of the new infectious diseases that cropped up in that time period.
Human contact with wildlife species that facilitate the transmission of novel viruses may increase in the future, as the population grows and humans searching for places to live and farm fan out to areas inhabited by or closer to wildlife.
Predicting the future
Stephen Morse, an epidemiologist at Columbia University, was in the early years of his career when the first case of HIV/AIDS was detected in the United States in 1981. In a pandemic that continues to this day, HIV, believed to have originated in chimpanzees, has infected 60 million people and caused an estimated 30 million deaths. [5 Scariest Disease Outbreaks of the Past Century]
"For many years, there was complacency, thinking that infectious diseases were pretty much becoming ancient history," said Morse, who studies how pathogens develop the ability to infect humans.
The kind of complacency present in those pre-HIV years largely no longer exists. Scientists are constantly on the lookout for the next pathogen that may cause an epidemic. One of the viruses that scientists have thought posed the greatest pandemic threat is the bird flu, or H5N1, a strain of influenza virus that has been circulating in birds and killing them. Resources devoted to prepare for and combat a bird flu pandemic in humans were shifted and applied to the swine flu pandemic in 2009.
Another worrisome influenza virus on the watch list is H7N9, an avian flu first detected in China in 2013 that has infected a number of people who had come in contact with infected birds. As viruses constantly change, it is also possible for them to mutate in a way that allows them to easily spread among people. In fact, one of the hardest questions for the scientists to solve is not just how viruses living in animals become able to infect humans, but also what makes them able to move from person to person, Morse said.
For H5N1, scientists have shown that the virus needs only four mutations to be able to transmit via air among mammals.
"With H5N1 and H7N9, we do a lot of worrying and watching, because we really don't know what to look for until it begins taking off in people," Morse said. "And at that point, it's already too late."
Morse and his colleagues are working on a project called PREDICT, part of the Emerging Pandemic Threat program run by the U.S. Agency for International Development, to help anticipate the next big disease threat.
"The idea is to see how early we can identify potential infections that could be serious, like the next SARS," Morse told LiveScience, calling from Uganda, one of the focus countries of the PREDICT program, where scientists monitor wildlife and people in contact with wildlife to discover novel pathogens.
"We are trying to understand more about the ecology of these infections, and what pathogens that wildlife species carry are likely to come into contact with human," he said.
Scientists have found that new viruses are more likely to surface in some parts of the world than others. Tropical Africa, Latin America and Asia are the disease emergence hotspots, and their high biodiversity and increasing human interaction with the environment may be helping viruses to make the leap into humans. And from there, they can go anywhere on the globe.
Epidemics may grow faster and cost more
Today, travelers are just a few hours' flight away from places that would have taken months to travel to by ground or sea in the past. This is a boon not just to humans, but to the microbes they carry. Sick travelers can introduce pathogens to new people as they travel, and at their destination, before they even realize they are sick. With future population growth, simple math suggests that there's going to be more travelers, potentially helping epidemics grow by quickly spreading the contagion.
"We're going to see connectivity between people increase, so there's more risk of a disease emerging in remote parts of the Amazon, and actually getting into our global travel network and affecting those in London, Moscow and Delhi," Daszak said.
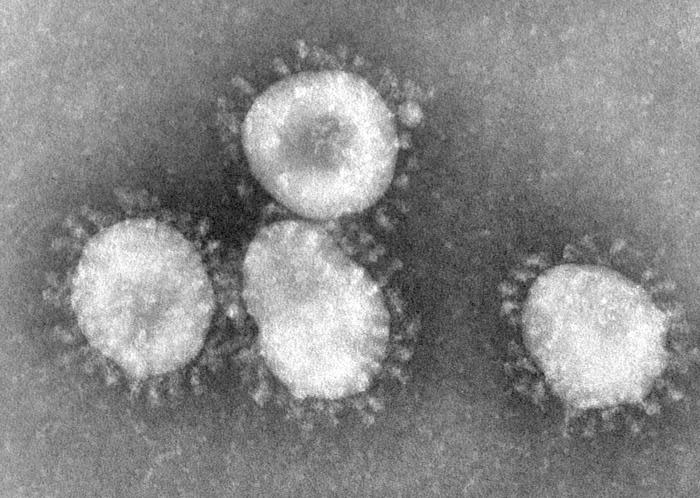
The emergence of SARS in 2002 in China painted a picture of what it would be like when a virus finds its way into the travel network: The virus rapidly propagated around the world in just a few weeks, infecting more than 8,000 people and killing about 800 before it was brought under control by limiting unnecessary travel and quarantining those affected.
A traveling virus may also cause economic damage, beyond even the costs associated with disease treatment and control. SARS cost billions of dollars by cutting international travel by 50 to 70 percent, and affected businesses in several sectors. Growth of the Chinese GDP fell by 2 percentage points in one quarter, and half a percentage point in annual growth, according to the World Bank and the Chinese government’s estimations. Is humanity prepared to face the future?
The movement of the world's population from sparsely populated rural areas to dense cities may also impact the spread of pathogens. By the year 2050, 85 percent of people in the developed world and 54 percent of those in the developing world are expected to have left rural areas for cities, according to United Nations' estimates.
From a global disease-fighting perspective, urbanization can have some positive effects. Better communication systems can help spread early warnings and other critical information at times of outbreaks. Moreover, better disease surveillance systems can be set up in urban settings compared with remote rural areas.
However, concentrated populations in cities may need a stronger public health sector to protect them.
People in crowded cities are often more vulnerable to infectious disease, especially in the face of natural disasters such as hurricanes and floods, which have particular public health problems associated with them, said Dr. Ali S. Khan, director of the CDC's Office of Public Health Preparedness.
"We are going to need a robust public health system to respond to population increase, urbanization, the aging population and increased travel, increased interaction between humans and animals that give rise to new diseases," Khan said.
But instead, "we've hollowed out public health, and I think this poses a great threat to the health security of our nation and global communities," he said.

The U.S. public health sector is suffering budget cuts at both the state and federal levels. Khan said the CDC's $1 billion program supporting disease identification and emergency operations now runs on $600 million, and with 45,700 fewer public health workers in the field, functioning as the eyes and ears of the agency.
However, the news isn't all gloomy, Khan said. "It is pretty clear that as we concentrate people in the city, there's an increase in creativity. So I'm optimistic that this increased creativity will lead to novel solutions that will help us identify disease, prevent and track better than we've ever been able to do in the past," he told LiveScience.
And there have already been glimpses of progress nowadays, Khan said, noting the rapid response by the CDC, WHO and other public health organizations to recently emerging viruses such as MERS, as well as the agencies' enhanced communication with the public.
"So think about all this great work where we look at social media to try to understand when a disease is emerging in the community, and we use social media to communicate with people in a way we were never able before," Khan said.
There has also been progress in developing novel diagnostics that can quickly detect infection before a person starts showing symptoms, and in sequencing genetic material of a pathogen to understand what it is and how it works, Khan said.
"Immense progress" has also been made in reducing the amount of time it takes to make a vaccine, Khan said. About two months after the 2009 swine flu pandemic was announced by the WHO, vaccines had been developed and production of enormous quantities of them were underway.
"We should expect to see a continuous acceleration of progresses, but this is not a given," Khan said. "I think people nowadays have a false sense of security, and I think part of this is that public health is working,” but that can only last so long if public health resources keep decreasing instead of strengthening, he said.
"We have eradicated and eliminated some diseases from our community, but the honest truth is most diseases don't get eliminated," Khan said. "Most diseases come home to stay."
Email Bahar Gholipour. Follow us @livescience, Facebook & Google+. Original article on Live Science.

Flu: Facts about seasonal influenza and bird flu
What is hantavirus? The rare but deadly respiratory illness spread by rodents









