New MRSA Superbug Emerges in Brazilian Patient
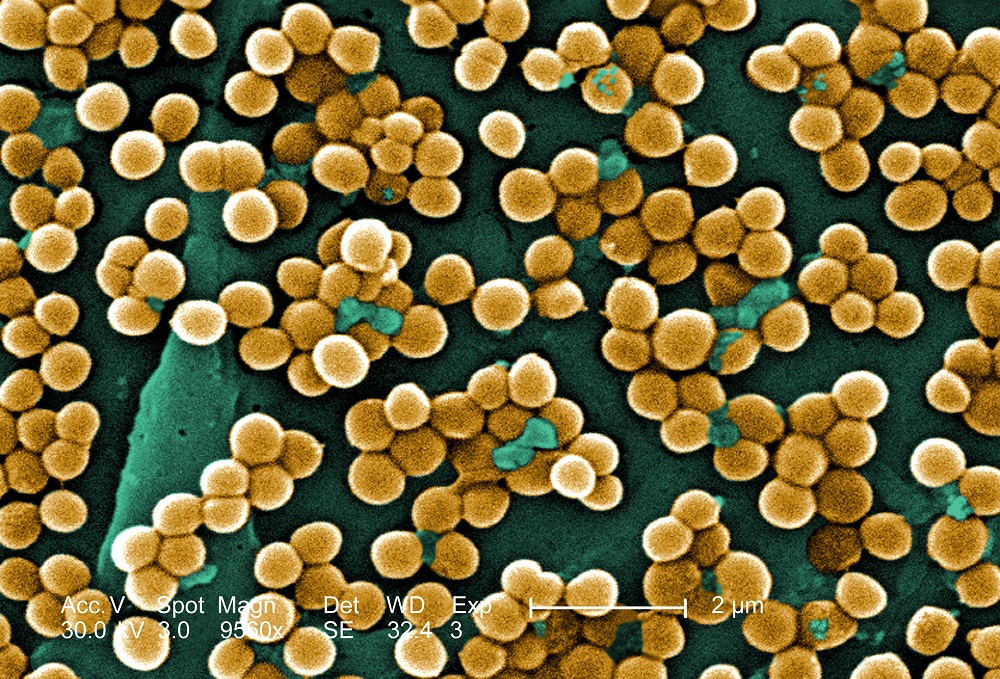
A new, highly drug-resistant type of the superbug methicillin-resistant Staphylococcus aureus (MRSA) recently caused a fatal blood infection in a Brazilian patient, according to a new report.
The 35-year-old man, who was in poor health and had been in the hospital for a long time, was infected with a strain of MRSA that developed resistance — during his hospital stay — to the powerful antibiotic vancomycin, which is widely used to treat this infection.
Researchers found that unlike previous superbugs that were associated with hospitals, this vancomycin-resistant staph bacteria (VRSA) is genetically related to a MRSA strain that has been circulating in the United States and northern South America, according to the study, published today (April 17) in the New England Journal of Medicine.
"This particular bug is genetically different from all the others that have been described before, and belongs to a clone that has been described before to cause infections in the community, and not in the hospital," said study researcher Dr. Cesar Arias, an infectious diseases scientist and an associate professor of medicine at the University of Texas.
These findings in the Brazilian patient's case "raise concerns that this particularly resistant contaminant can actually disseminate now much more easily than previously thought," Arias told Live Science. [7 Devastating Infectious Diseases]
Why the case was unique
MRSA is one of the most common causes of infections worldwide. It can cause a variety of infections, ranging from a simple skin boil to a nasty flesh-eating infection that can be fatal. Studies show that about one in three people carry staph bacteria in their nose, but it usually doesn't cause any illness. Two in 100 people carry MRSA, according to the Centers for Disease Control and Prevention.
Get the world’s most fascinating discoveries delivered straight to your inbox.
The cheapest and most commonly used drug to treat an MRSA infection is the antibiotic vancomycin. However, in 2002, a staph infection that was resistant to vancomycin was reported, and about 10 more cases were documented since, mostly in the United States.
But all of these reported cases were skin infections; the Brazilian man's infection was much more serious.
"The difference with this bug is that this is the first time the bug has been shown to be causing a bloodstream, aggressive infection in a patient," showing that acquiring resistance to vancomycin doesn't make the bacteria any less capable of invading the blood, Arias said.
How did it happen?
Researchers found that in the Brazilian patient, MRSA likely became vancomycin-resistant during the time the patient was being treated in the hospital with antibiotics, suggesting he didn't get this fully resistant bacteria from outside.
To become resistant to vancomycin, staph bacteria need a new piece of DNA transferred to them from another type of bacteria that is already resistant. Previous studies have found the vancomycin-resistance genes come from another bacterium called Enterococcus, which usually affects very sick people. These genes can be transferred between bacteria very easily both in the laboratory and in the patient's body.
"Bacteria have these pieces of DNA that can move from one to another — it's basically bacterial sex, and they do it a lot. They are very promiscuous," Arias said.
Researchers said there likely was an exchange of genes between some Enterococci and some staph bacteria within the man when he was infected with both bacteria. This exchange made the staph bugs resistant to vancomycin.
Moreover, in the lab studies, researchers found that when the gene was transferred, it could be passed easily from one staph bacterium to another.
"So, there is a strain of staph that has shown before that it can disseminate easily in the community, and has a genetic element that can also be transferred very easily, setting the stage for a breakout," he said.
Nowhere is too far
There's not enough data for scientists to know exactly how commonly MRSA is found in the Brazilian population, or whether other instances of vancomycin-resistance have happened. "This bug could sit happily in people who are perfectly healthy; we don't know if it's already out or not," Arias said.
But if the vancomycin-resistant superbug were to break out, it wouldn't stay confined to one region or country. [5 Scariest Disease Outbreaks of the Past Century]
"Bugs don't have passports. They don't respect borders. They can travel very easily," Arias said. "And, in fact, this has been shown for MRSA."
There are other drugs available to treat MRSA that have become resistant to vancomycin. However, all of the alternatives are much more expensive than vancomycin, and haven't been around as long, so less is known about them.
"Treating vancomycin-resistant staph would be much more complicated and much more expensive," Arias said. "If it happens in a developing country, it would break the health system."
Email Bahar Gholipour. Follow us @LiveScience, Facebook & Google+. Original article on Live Science.

 Live Science Plus
Live Science Plus





