How Science Is Outwitting Antibiotic Resistance

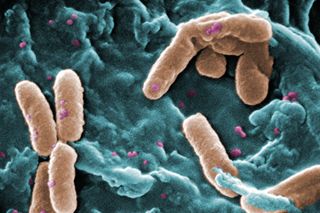
Antibiotics save countless lives and are among the most commonly prescribed drugs. But the bacteria and other microbes they're designed to eradicate can evolve ways to evade the drugs. This antibiotic resistance, which is on the rise due to an array of factors, can make certain infections difficult — and sometimes impossible — to treat.
Here are a few examples of how scientists funded by the National Institutes of Health are working to combat antibiotic resistance, from efforts to discover potential new antibiotics to studies seeking more effective ways of using existing ones.
Plumbing the Ocean Depths for New Antibiotics
Most antibiotics are derived from natural molecules that bacteria and fungi living in the soil and on plants produce to compete for limited resources. The ocean, too, is a rich source of microbes that could yield infection-fighting natural products. But it can be difficult to grow marine bacteria in the lab and coax them to produce their full repertoire of potentially therapeutic molecules.
A team led by Bradley Moore of the University of California, San Diego, developed a genetic approach to overcome these challenges and used it to discover a novel antibiotic compound. Working with a marine bacterium from ocean-floor sediments, the scientists first identified a cluster of genes predicted to make a natural antibiotic. Then, they clipped out the gene cluster and inserted it into a specially engineered, circular piece of DNA called a plasmid. Finally, they transferred the plasmid carrying the antibiotic genes into an easily grown bacterial species, which then produced the new antibiotic.
In lab tests, this antibiotic, named taromycin A, impaired the growth of several types of drug-resistant bacteria. Now that he and his colleagues have shown that the approach works, Moore says that they “hope to exploit it to fundamentally change the way naturally occurring antibiotic compounds are discovered and developed into new drugs.”
Breaking Down the Walls of Resistance
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Penicillin and other antibiotics in a class called beta-lactams kill bacteria by preventing them from making a mesh-like polymer that forms their cell wall — a structure critical to the cell’s survival. As bacterial cells grow and divide, they constantly rebuild and remodel their cell walls. Fragments from torn-down sections are recycled to form new cell-wall-building materials.
Beta-lactam antibiotics work by preventing bacteria from keeping up with the necessary cell-wall building and repairs, explains Shahriar Mobashery of the University of Notre Dame. However, bacteria have evolved ways to fight back. For example, some of the cell-wall fragments that accumulate as a result of the drug’s damage can trigger a cascade of biochemical events culminating in destruction of the beta-lactam antibiotic. This vigorous resistance response has reduced the effectiveness of beta-lactams in fighting a range of infections.
Mobashery is studying cell-wall recycling and the effects of beta-lactams on this process in the bacterium <i>Pseudomonas aeruginosa</i>, a common cause of infections in hospitals and other health care settings. By uncovering the step-by-step details of the recycling process and identifying molecules that trigger resistance, he hopes to find new antibiotic targets that are less likely to be circumvented by microbial evolution.
Using Today’s Antibiotics More Wisely
Another way to combat resistance is to improve how we use existing antibiotics. Ever since the advent of penicillin in the 1940s, most scientists and physicians have believed that the best way to minimize the emergence of resistance is to wipe out all the bacteria in an infection as fast as possible. That’s why doctors stress the importance of taking all of the pills they prescribe for these ills, even after symptoms subside. But Andrew Read of Penn State University is not convinced that this approach is best. Today’s treatment regimens, he says, “are a double-edged sword.” He explains that if an infection already contains some drug-resistant microbes, aggressive therapy such as long or high-dose regimens could rapidly eliminate microbes that are susceptible to the drug, leaving behind resistant ones. These resistant microbes could then flourish and spread through a hospital or community.
Using malaria-infected mice as a model system, Read is investigating whether alternative treatment regimens could help slow the evolution and spread of resistance and prolong a drug’s useful life. Like bacteria, malaria-causing parasites are continually evolving ways to evade the drugs designed to eliminate them. Read’s findings indicate that “lighter touch” drug regimens that get rid of an infection more slowly do a better job of controlling the spread of resistant organisms in a population while also restoring health to individuals and keeping them from being contagious.
It remains to be seen whether these observations will hold true for human infections. “What we need is a lot more case-by-case analysis” of how best to treat each disease, Read says, noting that combinations of drugs could also help thwart resistance. Until we know the answers, he emphasizes, people should follow what their health care providers say when taking medicines to treat infections.
This Inside Life Science article was provided to Live Science in cooperation with the National Institute of General Medical Sciences, part of the National Institutes of Health.
Learn more:
Antimicrobial Resistance: Global Report on Surveillance 2014
Also in this series:
Most Popular