Immunotherapy: Could the Human Body Be Trained to Fight Cancer?
This article was originally published at The Conversation. The publication contributed the article to Live Science's Expert Voices: Op-Ed & Insights.
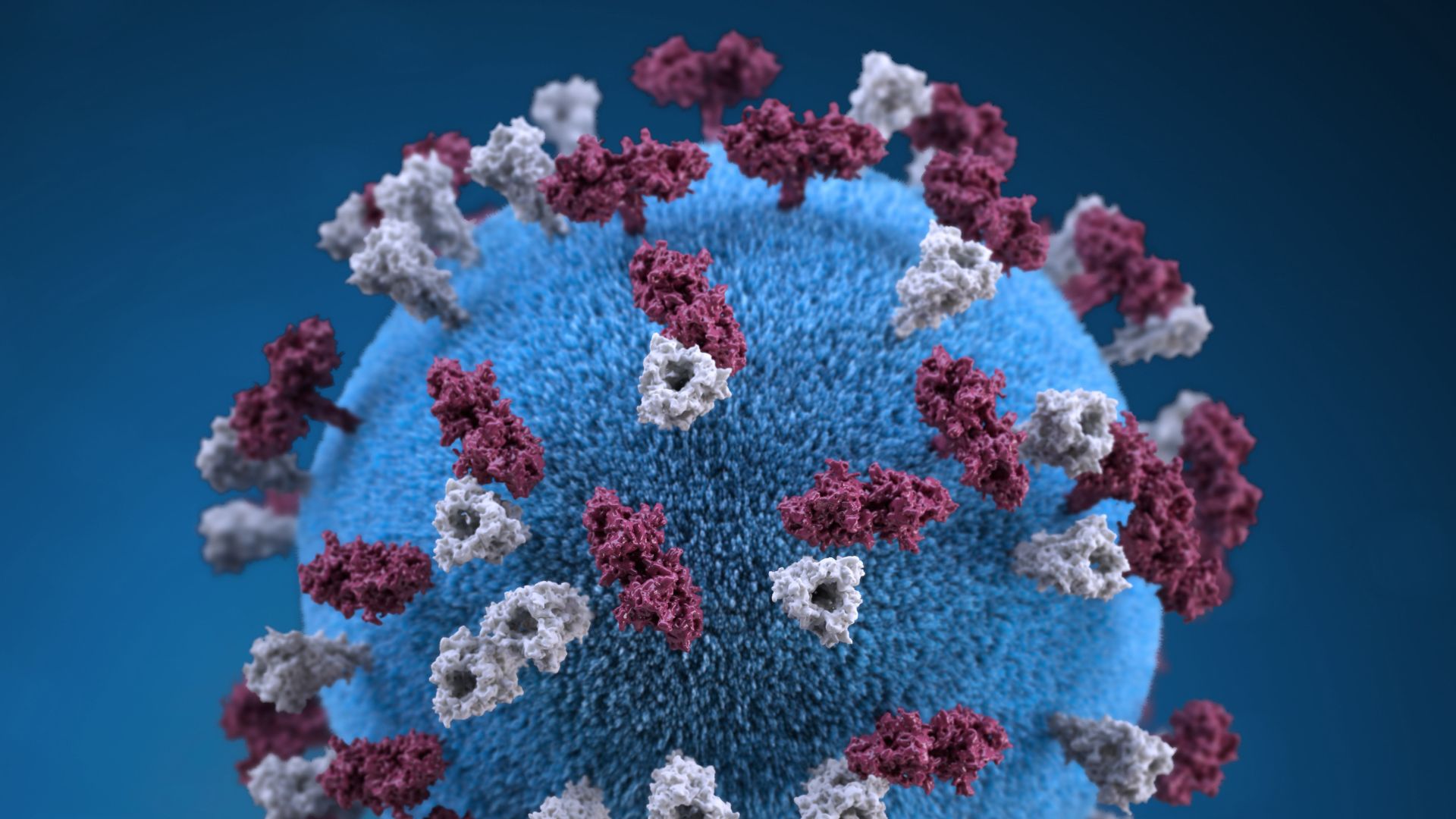
The human immune system is powerful and complex.
It can identify and destroy invaders of nearly infinite variety, yet spare the more than 30 trillion cells of the healthy body.
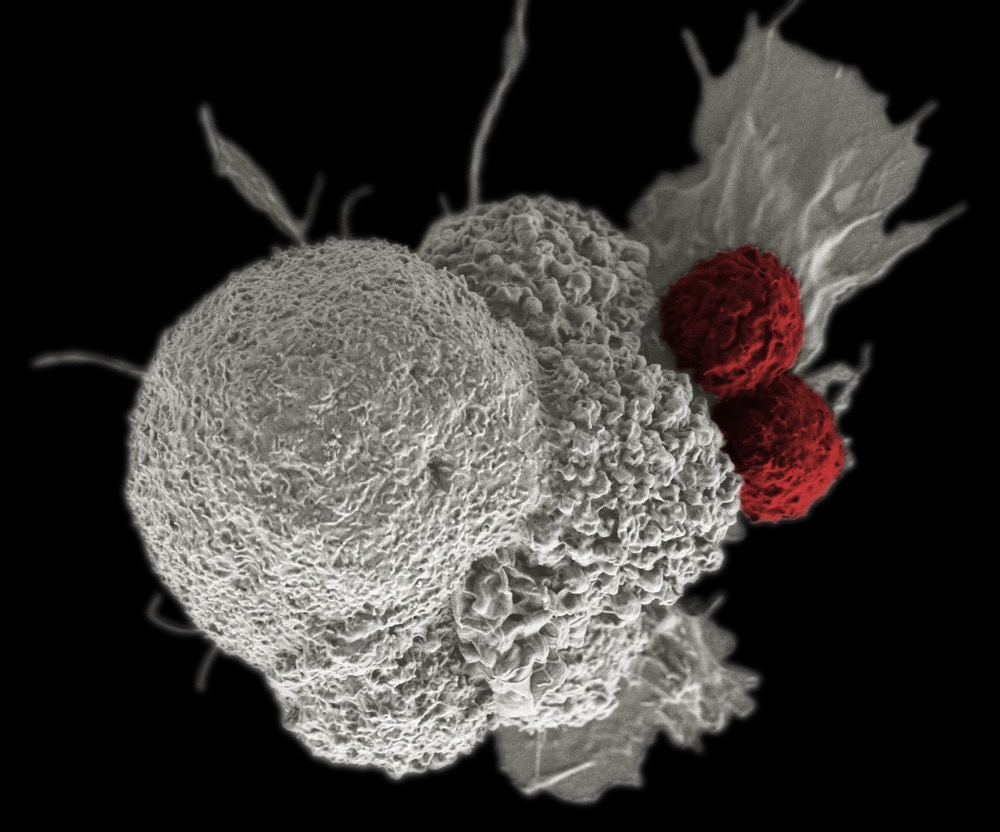
Unfortunately, the broken cells of cancer are able to retain, and boost, the "recognize and ignore me" signals of undamaged cells, letting them evade detection by the immune system. As a result, these damaged cells grow unmolested, destroying the normal physiological functioning of tissues and organs.
Armed with new insights into the interactions between cancer and the immune system, research teams are developing novel treatments to harness the full potential of the body’s natural defenses. This is called immunotherapy.
In animal models and clinical trials, breakthrough immunotherapies are emerging, techniques that train the immune system to recognize and attack cancer as the enemy.
One way is through drugs that help the immune system find and destroy cancer cells. Another way is through vaccines that can teach the body to recognize cancer cells.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Recently, studies have paired immunotherapies with modified viruses that attack tumor cells and keep them from returning.
With promising results, such new weapons are providing hope that cancer can ultimately be defeated.
Harnessing the immune system
When foreign cells – like viruses or bacteria – infect the body, the immune system springs into action. It produces antibodies that bind to proteins called antigens on the surface of the foreign cell. Sometimes this is enough to neutralize the foreign cell. In other cases the antibodies bind to the antigen and mark the cell for destruction by T-cells, or both.
Cancer cells also produce antigens. But even though cancer cells are not normal and would otherwise be marked for destruction, antibodies don’t bind to their antigens and the immune system does not destroy them. This is because cancer cells have evolved to hijack normal protective checkpoints in the immune system to protect themselves from elimination.
Cancer cells ramp up those barricades to stay shielded and simultaneously weaken immune cells. This allows them to grow unchecked, developing blood vessels and invading into other tissues.
Immunotherapies can "educate" the immune system to produce antibodies that can bind to the antigens on cancer cells, and thus block the growth-promoting function of these antigenic proteins or flag them for recognition and destruction by immune cells.
Using drugs to stimulate the immune system
One promising group of immunotherapy drugs are laboratory-made monoclonal antibodies. These drugs can bind to cancer cell antigens and mark them for death.
For example, trastuzumab (Herceptin) is a monoclonal antibody that binds to an antigen human epidermal growth factor receptor-2 (HER-2) that is found in abundance on some of the most deadly breast cancers. Herceptin binding triggers an immune assault on the breast cancer cells.
In addition to antigens, the surfaces of cancer cells also have "normal" proteins. These proteins can "silence" the immune system, and prevent T-cells from destroying the cancer cell. Monoclonal antibodies can recognize these "normal" proteins and block them.
While antibody-mediated therapy has shown promise, such drugs are not always a cure, and with a price tag well over US $100,000, can be a huge burden on the patients and their families.
Using vaccines to fight cancer cells
One approach that we are studying at The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute and in institutions across the globe is to develop single-shot vaccines that trigger the same processes.
The idea is that vaccination or immunization with carefully engineered synthetic proteins can train the immune system to recognize antigens on cancer cells, effectively inoculating a patient against a cancer for years at a time. And, the treatment should cost far less than $1,000 per patient.
There are several approaches in process, such as a HER-2 breast cancer vaccine, which we are evaluating in Phase II trials.
Such vaccines, if ultimately successful, could also be paired with checkpoint inhibitors to create an even more favorable environment for T cells to do their work.
The approach mimics the effect of monoclonal antibodies, but with a more direct, and much more cost-effective, technique. Instead of receiving antibodies, the patients themselves make the antibodies through the vaccination process.
In our trial, patients (who were all terminally ill) developed antibodies against their cancers via the vaccine. Ten patients out of 24 (41 percent) enrolled in the trial fought their cancer well enough to come back for a six-month booster. One patient has survived more than three years, and our hope is that by administering the vaccine earlier in a patient’s treatment, before the immune system is compromised by chemotherapy and radiation, the impacts will be even more profound.
To date, the treatment appears to show no toxicity and minimal side effects.
Unleashing a viral army
Researchers are also co-opting the intricacies of infection to assault cancer.
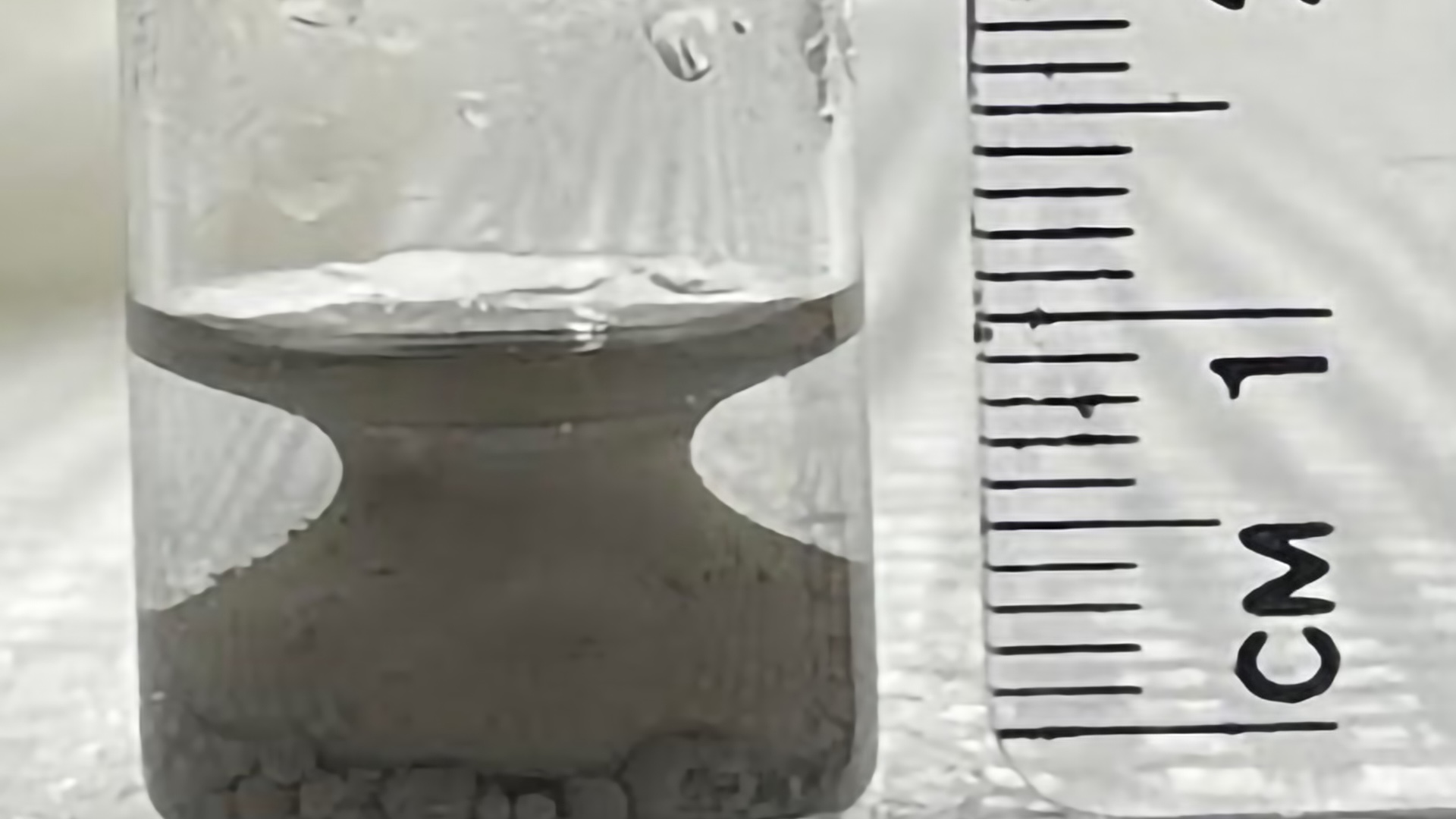
Most powerfully, we are realizing that viruses can be trained to attack cancer, with a dual benefit. First these viruses, called oncolytic viruses, can directly assault tumor cells, and they can also massively replicate within the diseased cells, causing them to violently explode. The ensuing tumor destruction recruits the body’s immune cells, now enabled to recognize cancer cells, to attack the cancer cells with every tool in their arsenal.
Just as with immunotherapy vaccines, oncolytic viral therapy can create a long-term, robust defense that trains the immune system to attack cancer over months, or even years.
Current work at the OSUCCC-James using oncolytic viruses takes advantage of three categories of treatment – a virus, a cancer drug and an immunotherapy – to treat a deadly form of brain cancer called glioblastoma.
We matched a modified oncolytic herpes simplex virus with a drug called bortezomib (which slows tumor growth and boosts the impact of radiation and chemotherapy) and an immunotherapy, which in this case is an infusion of immune cells.
In that study, bortezomib and the modified herpes virus tore apart tumor cells via a process called necroptosis. In turn this triggered the release of inflammatory molecules that redirected the efforts of cancer-killing immune cells to recognize and eradicate the cancer threat. In our animal model, the added infusion of natural killer cells helped eradicate tumor remnants.
The future of immunotherapy
As immunotherapies evolve, they will grow more effective, with combination therapies bringing every available treatment to bear when cancer strikes.
However, there are limitations. Immunotherapy treatments are not "one size fits all." Different patients will respond better to different treatments, and some cancers may not respond at all. Identifying specific changes in tissue that can be monitored, called biomarkers, to predict which patients are likely to benefit from a particular treatment strategy would be a game-changer for future personalized therapy.
What we need are continued efforts to identify such biomarkers to personalize treatment selection for each patient. Current technology is also limited in that it cannot yet produce large quantities of vaccine or create potent oncolytic viruses in high concentrations. Engineering more powerful next-generation viruses in a cost-effective manner and in large concentrations remains a necessary goal.
However, the biggest challenge in viral and immunotherapy is to walk that razor edge to harness the good to destroy cancer without having the potential toxicity that can become lethal and destroy nonmalignant cells.
While we all strive for a cancer cure, and the outcomes from initial studies and trials truly seem miraculous at times, we must first do no harm. We remain inspired that medical research advances with knowledge, and that our knowledge is growing.
Balveen Kaur, Professor, OSU Comprehensive Cancer Center, The Ohio State University and Pravin Kaumaya, Professor, OSU Comprehensive Cancer Center, The Ohio State University