Long COVID: 3 years on, here's what we know so far
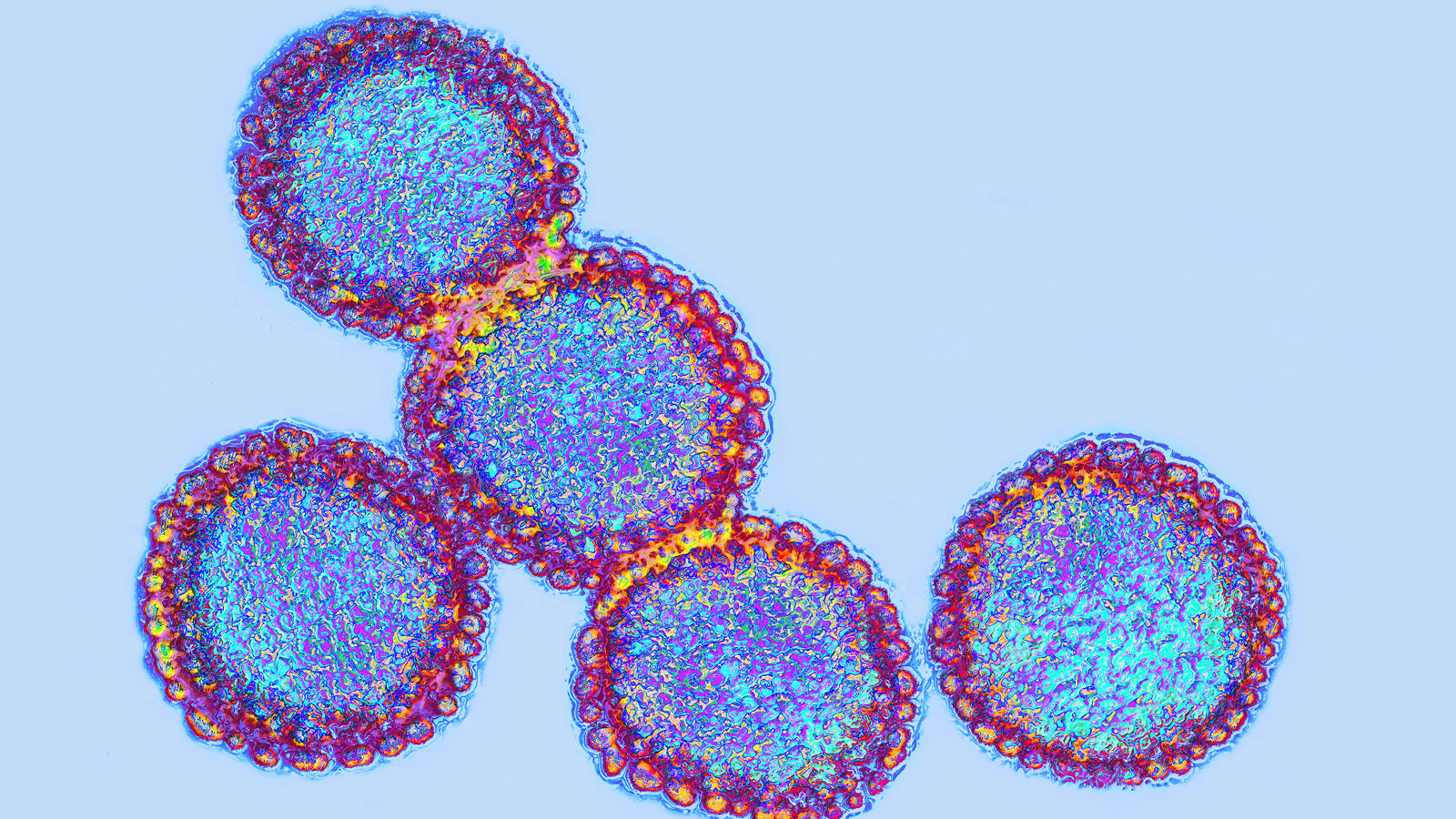
Researchers are beginning to understand some of the potential causes of long COVID and are investigating treatments for the complex condition.

Long COVID is a complex condition that is still not fully understood. According to the Department of Health and Human Services, the working definition of long COVID is "signs, symptoms and conditions that continue or develop after initial COVID-19 or SARS-CoV-2 infection." These can affect many organ systems and last for weeks, months or even years.
Dr. Maureen Baker, the chief medical officer at digital care platform Healthily and the former chair of the Royal College of General Practitioners in the U.K., told Live Science that understanding what causes long COVID is crucial to helping people manage their symptoms.
"Why do some people develop long COVID while others do not? The answer to this question is not yet clear," she said. "There are likely multiple, potentially overlapping causes of long COVID, so the underlying reasons for the illness are likely to be different for different people."
Experts still don't understand why this condition happens, but thanks to an intense global research effort, they are getting closer to finding answers. Three years on from the start of the COVID-19 pandemic, here's what we know about long COVID so far.
What are the symptoms of long COVID?
Patients with long COVID report a wide range of symptoms and conditions that can have a debilitating impact on both physical and mental health, according to a landmark 2023 review published in the journal Nature Reviews Microbiology. Researchers have identified more than 200 symptoms across multiple organ systems, with the onset and timing of symptoms differing between individuals.
According to the Center for Disease Control and Prevention (CDC), common symptoms of long COVID include:
- Tiredness or fatigue
- Post-exertional malaise (symptoms that get worse after physical or mental effort)
- Fever
- Cardiorespiratory problems, such as cough and heart palpitations
- Neurological symptoms, such as memory loss and sleep problems
- Digestive symptoms, such as abdominal pain and diarrhea
- Muscle and joint pain

Long COVID can also significantly impact a person's mental health. Some individuals may experience trauma and distress from ongoing symptoms, said Catherine Tregoning, a chartered health psychologist and a mental health officer at the U.K.-based Autoimmune and Support Awareness Foundation, a nonprofit aimed at improving awareness and reducing the isolation of those with autoimmune conditions.
"Those who have been affected by long COVID can be understandably concerned about catching COVID again, worry about their long-term health and find it difficult to cope with their symptoms," Tregoning told Live Science in an email. "This can result in low mood, and stress and anxiety behaviours like difficulty sleeping, irritability and easily feeling overwhelmed."
It may be possible to group long COVID symptoms into four different subphenotypes, or clusters, according to a 2022 study published in the journal Nature Medicine. These clusters are:
- Cardiac and renal (kidney-related)
- Respiratory, sleep and anxiety
- Musculoskeletal and nervous system
- Digestive and respiratory system
Each cluster was linked with distinct patient demographics, underlying health conditions and SARS-CoV-2 infection severity. For example, Baker said, women were more likely to be affected by respiratory and sleep problems.
The review researchers believe this way of categorizing symptoms could enable more targeted long-COVID treatments. However, more research is needed to understand how this discovery may be applied in clinical practice, particularly in relation to patients who may not neatly fall into one of these subcategories.
What causes long COVID?
There are likely multiple causes of long COVID, according to the Nature Reviews Microbiology review.
Immune dysregulation
One of the main features of long COVID is severe dysregulation of the immune system – meaning when the body can't control or sustain an immune response. According to the Nature Reviews Microbiology review, studies have shown that the illness can cause alterations to the number and functioning of white blood cells (responsible for fighting infections and destroying cancerous tissues) and interferons (proteins released by host cells to alert other cells of potential danger).
Scientists have also suggested that the body's inability to clear itself of the virus could be a driver of long COVID symptoms. Viral proteins have been found in numerous organs, including the brain, muscles, lymph nodes, liver and blood plasma, weeks and even months after the initial infection, the review noted.
In addition, many researchers point to the similarity between long COVID and chronic fatigue syndrome (CFS), a condition previously linked to immune dysregulation.
"Chronic fatigue is a condition of extreme fatigue in someone present for more than six months, accompanied by post-exertional malaise," said Dr. Deepak Ravindran, co-founder of the Berkshire Long COVID Integrated Service in England. In many patients, it presents after a viral illness, Ravindran told Live Science in an email.
"There are many similarities between long COVID symptoms and chronic fatigue symptoms, including fatigue, brain fog, aches and pains, stomach disturbances, chest pain and irregular heart rates," Ravindran said. "The present understanding is that there is likely to be some underlying mechanisms that are similar to both conditions."
Circulatory system disruption
Patients with long COVID may have impaired blood clotting and problems with circulation, according to a 2021 study published in the journal Frontiers in Cardiovascular Medicine and a 2022 study published in the journal Cardiovascular Diabetology.
"These clots can form in the small blood vessels in the lungs, leading to scarring, which can impair blood flow and reduce lung capacity," Baker said.
Researchers also found that long COVID can promote inflammation of the heart muscle and cause dysfunction in the cells that line blood vessels, leading to a narrowing of the arteries that may lead to chest pain and high blood pressure, according to the Nature Reviews Microbiology review.
Neurological and cognitive systems
Scientists are not sure what causes long COVID's neurological symptoms, nor whether they are all caused by the same mechanisms, said Maxime Taquet, a senior research fellow at the University of Oxford in England who is investigating neurological and psychiatric outcomes of long COVID.
One hypothesis is that SARS-CoV-2 triggers inflammation in many different parts of the body, which can include the brain, Taquet told Live Science over email. Other hypotheses include the formation of blood clots in the brain; the body attacking itself with antibodies; the virus staying hidden in pockets within the body and possibly the brain; and the virus reactivating dormant infections such as Epstein–Barr virus, the pathogen behind "mono," he said.
Long COVID may also be linked to the loss of nerve fibers in the eyes, according to a 2022 study published in The British Journal of Ophthalmology.

What are the risk factors for long COVID?
Scientists are still unsure exactly what puts someone at risk of long COVID, Taquet said.
"We can speculate that some of it has to do with the severity of the illness," he said, and a 2021 retrospective study in the journal PLoS Medicine found that people who initially had severe COVID-19 infections were more likely to develop long COVID.
However, Ravindran said that patients seem to respond differently. "We thought that more severe cases of acute COVID will be left with long COVID, but we are finding that a lot more patients have had mild versions of COVID before going on to have very severe symptoms of long COVID," he said. "This is very new and very different to our usual understanding of infectious diseases."
Whether the severity of the infection plays a role in long COVID is yet to be determined, according to the Nature Reviews Microbiology. Researchers estimated the incidence of long COVID at 10 % to 30% among non-hospitalized cases and 50% to 70% among hospitalized cases of COVID-19.

The SARS-CoV-2 variant someone is infected with may also be a factor, Taquet found in a 2022 study. "The delta variant caused more neurological conditions than omicron," he noted, "And some of it has to do with the patient themselves."
According to the Nature Reviews Microbiology review, medical conditions that may make a person more likely to get long COVID include type 2 diabetes, connective tissue disorders, attention deficit hyperactivity disorder (ADHD) and chronic urticaria (a raised, itchy rash). However, the review authors noted that a third of people with long COVID have no identified pre-existing conditions.
Understanding more about who is at risk of getting long COVID is important for putting the right prevention strategies in place, Ravindran said.
How is long COVID diagnosed?
Dr. Stuart Katz, an investigator at Researching COVID to Enhance Recovery (RECOVER), a National Institutes of Health (NIH) research initiative, told Live Science in an email that diagnostic tools for long COVID are mostly still in development.
"Right now, there is no universal definition for long COVID, and this is because research is ongoing," he said. "The key to doing this is identifying biomarkers or biological indicators of disease. But before we can identify long COVID biomarkers, we need to collect, analyze, and test our data to help narrow down key disease characteristics."
According to the Nature Reviews Microbiology review, the current approach to diagnosis is largely symptom-based. Diagnostic tools may include imaging to detect blood clots, corneal microscopy to identify nerve damage in the eye, electrocardiograms to scan for heart damage, and use of hyperpolarized magnetic resonance imaging (MRI) to detect abnormal gas exchange in the lungs.
Can long COVID be prevented?
One of the best ways to protect against developing long COVID is to get vaccinated, Taquet said.
"It protects against COVID-19 in the first place and one of the best ways to avoid long COVID is to avoid COVID," he said. There is some evidence that among those with breakthrough infections — i.e. COVID-19 after being vaccinated — that the risk of long-term symptoms is lower, he added. According to the 2023 review, studies indicate that vaccines may provide partial protection, reducing the risk of having long COVID by 15% to 41%. These mixed results could be explained by differing study methods, time since vaccination and definitions of long COVID, as well as differing variants of the SARS-CoV-2 virus, researchers suggested.
More research is needed to understand which prevention strategies may be most effective.
Is long COVID treatable?
There are no known curative treatments for long COVID, but there are some ways to manage symptoms, Katz told Live Science.
According to the review in Nature Reviews Microbiology, pharmacological treatments for long COVID symptoms include:
- Intravenous immunoglobulins: Immunoglobulins, often referred to as antibodies, are proteins released by the immune system to identify and neutralize bacteria and viruses. Patients are given a cocktail of these through a drip into a vein to treat immune dysfunction.
- Low-dosage naltrexone: Medication primarily used for the treatment of alcohol and opioid use disorders and also prescribed off-label to treat some chronic pain and autoimmune conditions. This helps reduce inflammation within the nervous system, according to a 2014 review published in the journal Clinical Rheumatology.
- Beta-blockers: Medication prescribed for blood pressure and heart rate disruptions.
- Anticoagulants: Medications that prevent the formation of blood clots.
Other options include:
- Antihistamines: Medication used to relieve allergy symptoms such as running nose and congestion.
- Paxlovid: Antiviral medication used for treating COVID-19. Paxlovid reduces the mortality and hospitalization rates in patients with COVID-19, but it's unclear how effective this drug may be against long COVID symptoms, according to a 2022 meta-analysis published in the journal Annals of Medicine.
- Sulodexide: Medication used to treat vein and artery disorders. Preliminary study published in the journal Archives of Cardiovascular Diseases has shown that Sulodexide may help improve cardiovascular symptoms of long COVID.

A psychological approach to long COVID focuses on supporting patients to self-manage their physical and mental symptoms, Tregoning said.
"Stress management can reduce fatigue, relaxation techniques can help sleep disturbances and anxiety management can improve brain fog," she said. "Mental health teams provide strategies to help with pacing, pain management, panic attacks resulting from breathing issues and memory problems to name but a few."
Evidence is emerging that patients with long COVID may also benefit from occupational or physical therapy, when patients are prescribed activities designed to improve their balance, coordination, flexibility and strength, according to a 2022 review in the journal Viruses. Preliminary trials showed improvements in strength, respiratory function, physical fitness and quality of life, with no adverse side effects, such as increased fatigue or muscle pain. However, more studies are needed to determine which exercise protocols may be most effective. For example, exercise is currently not recommended for patients with long COVID who have chronic fatigue syndrome or post exertional malaise (the worsening of symptoms following even minor physical or mental exertion), according to Nature Reviews Microbiology.
This article is for informational purposes only and is not meant to offer medical advice.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.

Anna Gora is a health writer at Live Science, having previously worked across Coach, Fit&Well, T3, TechRadar and Tom's Guide. She is a certified personal trainer, nutritionist and health coach with nearly 10 years of professional experience. Anna holds a Bachelor's degree in Nutrition from the Warsaw University of Life Sciences, a Master’s degree in Nutrition, Physical Activity & Public Health from the University of Bristol, as well as various health coaching certificates. She is passionate about empowering people to live a healthy lifestyle and promoting the benefits of a plant-based diet.