Life-Threatening Bacteria Infection Remains Mysterious
About 250,000 Americans die each year from sepsis, a severe illness caused by the body's overwhelming immune response to infection. That's more than the number of U.S. deaths annually from prostate cancer, breast cancer and AIDS combined.
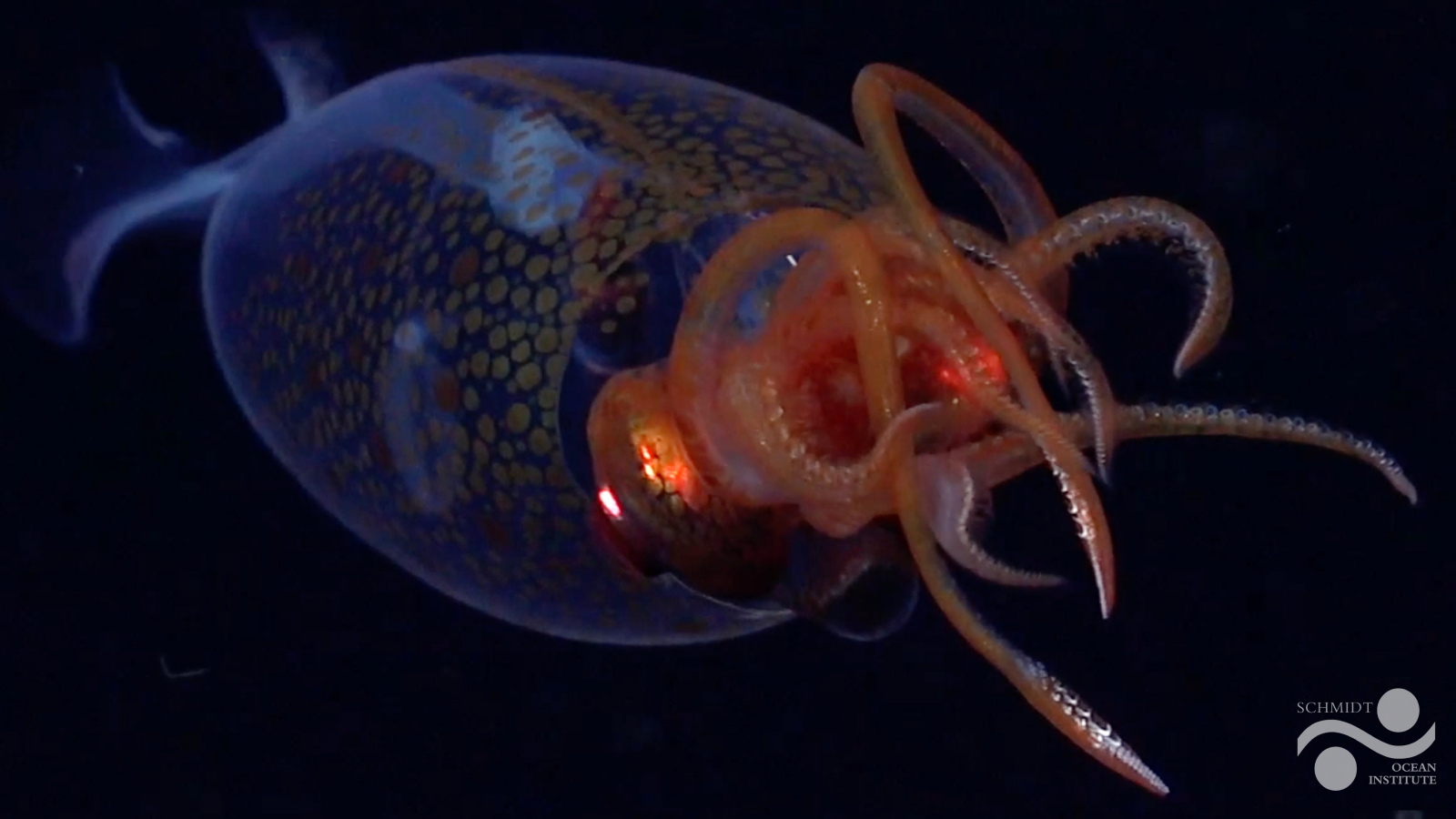
Sepsis typically stems from an infection, whether it starts in the lungs, urinary tract, the site of a medical device or elsewhere. The infection sends the immune system into overdrive. Like using a machine gun to kill a cockroach, the immune system fires its biological and chemical bullets throughout the body. Blood vessels, organs and eventually the entire body become inflamed. One by one, vital organs fail: the lungs, liver, kidneys and, in the worst cases, heart.
Sepsis can arise unpredictably and progress rapidly. While doctors use a variety of strategies to detect and treat the condition, sometimes it's too late to prevent dire outcomes. Part of the problem is that they still don’t have a clear understanding of the underlying biological processes that makes the immune system go haywire and trigger sepsis.
As with many diseases, sepsis likely stems from many factors. Researchers funded by the National Institutes of Health have followed different leads. Identifying all the possibilities will aid the ongoing search for new and more effective diagnostic tools and treatments.
NO Way Out
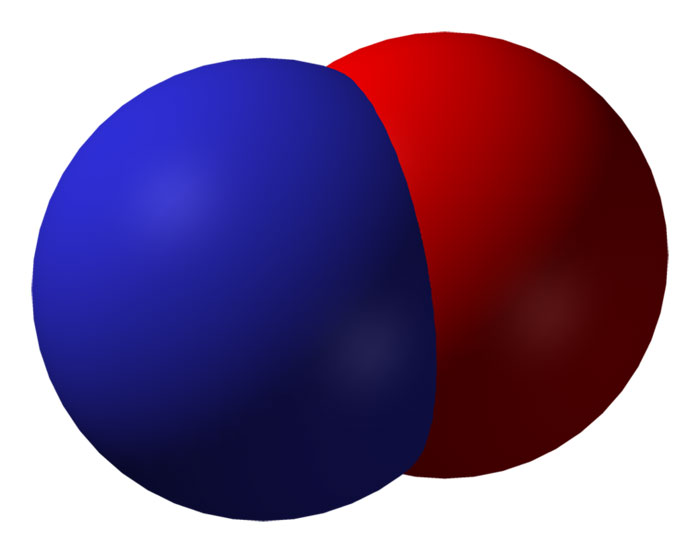
Veterinarian Cynthia Otto at the University of Pennsylvania in Philadelphia thinks that a gas called nitric oxide (NO) may be at the root of sepsis’s many complications.
In a healthy body, NO is an important chemical messenger produced by white blood cells called macrophages. It helps regulate blood pressure by opening blood vessels, and it defends against bacteria and other invaders. When macrophages encounter toxic bacterial products or when they’re deprived of oxygen—both of which occur in early sepsis—they ramp up production of the enzyme that makes NO. At high levels, NO can kill cells and inflame tissues.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Otto suspects that when sepsis starves tissues and organs of oxygen, it triggers a blast of NO that’s harmful instead of helpful. In experiments, she deprived cells of oxygen and then measured levels of NO and a related enzyme. The results showed a spike in their levels, suggesting that oxygen deprivation, as seen in people with sepsis, changes NO production and unleashes a severe immune response. This basic research finding provided a new lead for sepsis treatment involving inhaled NO that is now being tested in a clinical trial.
Cytokine Theory of Disease
Immunologist and neurosurgeon Kevin Tracey at New York’s Feinstein Institute for Medical Research focuses on one of the immune system’s foot-soldiers: proteins called cytokines that get released into an infected area to help heal wounds and repair damaged tissue. Previous research had suggested that a cytokine called TNF plays a role in fighting infection. Tracey thought it might also be involved in sepsis.
Through a series of animal experiments, Tracey showed that excess TNF triggered sepsis-like symptoms—and that a compound he developed could switch off TNF production and prevent sepsis from progressing to its most severe stage, called septic shock, in baboons. In a surprising finding, Tracey noticed that the compound seemed to work by powerfully affecting the nervous system. It turned out that the compound activated the vagus nerve, which runs from the brain stem down into internal organs and regulates heart rate, digestion and other essential functions. Stimulating the nerve with an electrical device dropped TNF production, resulting in less inflammation.
Since then, Tracey has shown in animals that stimulating the vagus nerve can block not only sepsis, but also arthritis, shock, heart failure and inflammation of the colon and pancreas. The foundation is now being laid to test some of these anti-TNF approaches in humans. Tracey is also investigating HMG-B1, another type of cytokine discovered in his lab that's likely involved in sepsis.
More Potential Culprits
Other scientists are looking elsewhere for the causes of sepsis.
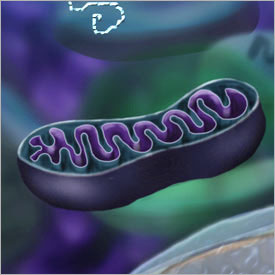
Trauma surgeon Carl Hauser at Beth Israel Deaconess Medical Center in Boston is investigating mitochondria. These cellular power plants can spill into the bloodstream after an injury. Because they're biologically similar to bacteria, free mitochondria can ignite a sepsis-like immune response.
At the Oklahoma Medical Research Foundation in Oklahoma City, cardiovascular biologist Charles Esmon points to histones, the spool-like structures that wind DNA into tidy shapes. Esmon found that histones can enter the bloodstream during an infection and cause sepsis. He also discovered that Xigris®, a drug used to certain sepsis cases, works by chopping up histones.
Learn more:
- Taking Aim at Sepsis: Fact Sheet
- Dogging Sepsis: Profile of Cynthia Otto
- For Janice: Profile of Kevin Tracey
This Inside Life Science article was provided to LiveScience in cooperation with the National Institute of General Medical Sciences, part of the National Institutes of Health.