Can a Vaccine Cure Haiti's Cholera?
The cholera epidemic in Haiti has cast a stark light on deep development holes and disagreements about whether a short-term patch—in the form of a cholera vaccine—can help in the long-term fight for better health.
A developing nation, Haiti has long struggled to maintain modern public-health projects. Even before the January 12, 2010 earthquake, the country was already falling behind. In 1990 more than a quarter of the population had access to sanitary facilities, but by 2008 only 17 percent of Haitians did. The earthquake brought further destruction to the country's limited infrastructure. Almost before the dust from the devastation settled, however, the international outpouring of support and aid seemed to signal a new opportunity to bring the most basic of health tools—clean water and decent sanitation—to Haitians.
Now, two years after the earthquake, Haiti is backsliding again. In the first half of 2010, about half of people in settlement camps in Port-au-Prince had clean drinking water, but by the end of the year only 7 percent did. And even as the cholera epidemic subsides to a couple hundred cases a day between rainy seasons, experts anticipate a spike in illness and deaths as soon as the rains return, starting next month.
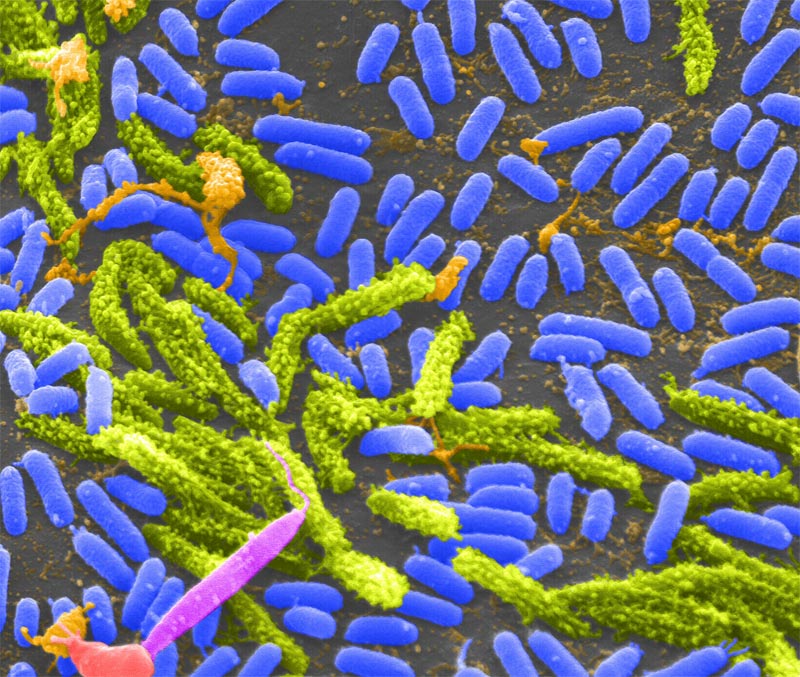
Since the first cases of cholera appeared in October 2010, some 7,000 people have died from the diarrheal disease (caused by the pathogen Vibrio cholerae, which is transmitted via unclean drinking water) and at least 520,000 have suffered symptoms. Treatment is simple (oral rehydration salts), and prevention is basic (clean drinking water and proper sanitation). But for impoverished Haiti, these solutions are still largely out of reach.
That is why many advocates argue for the distribution of the cholera vaccine, which has passed clinical trials and received approval by the World Health Organization (WHO) for global use. But many groups, such as the Pan-American Health Organization (PAHO), are taking a wait-and-see approach and are not yet ready to back a full rollout of the vaccine.
Prevention imperfect?
The two existing cholera vaccines, Dukoral and Shanchol, are taken orally in two doses two weeks apart, and immunity takes about a week to kick in and lasts for two or three years. They are about 60 to 90 percent effective.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Those at Partners In Health, a health care organization, say that imperfect efficacy should not matter in Haiti. "If you have a vaccine that was about 80 percent effective compared to 0 percent effective of drinking stool-laden water, which would you choose?" asks Paul Farmer, co-founder of the organization and a professor at Harvard University. "It's not as good as the polio vaccine, but neither is the flu vaccine." Indeed, the cholera vaccines are roughly as effective as flu vaccine, and are "pretty frickin' good," says Farmer. Shanchol has emerged as the favorite, as unlike Dukoral it does not need to be diluted with water.
Partners In Health is collaborating with the Haitian NGO Gheskio to start distributing Shanchol in two locations—in the rural area of Bocozel in the Artibonite River Valley and the more urban Port-au-Prince slum Cité de Dieu. They have 200,000 doses of Shanchol on order from the Indian manufacturer, Shantha Biotechnics, and hope to start the pilot program next month—although Farmer says they had hoped it would start last year.
PAHO, WHO and other organizations will be watching the program closely to see if the logistics of distribution pan out. "It needs to be verified in the field," says Andrea Vicari, a vaccination advisor at PAHO, of the vaccine program, explaining that although it has worked well in clinical trials and previous assays in Asia, on the ground, in Haiti, it might prove less effective because of gaps in distribution and people not taking both doses. Vicari plans to visit Haiti to assess the situation at the end of the month. Success could mean a green light for the rest of the country—and likely the world—to use these vaccines on a larger scale to provide immunity where cholera is endemic.
And Partners In Health is eager to show results. "The most immediate data we will have will be completion-rate data: Can we get two doses to the majority of the population we're targeting," says Jon Weigel, a researcher at Partners In Health. "We're not worried about whether it will be a safe or effective vaccine—we know it is. That data on completion rate will convince any skeptics about whether it can be rolled out on a wider scale in Haiti."
Dosage deficiency
The lack of access to clean water and proper sanitation facilities means that "we have to consider nearly everybody at risk in Haiti for developing cholera," David Olson, Doctors Without Borders medical advisor for diarrheal diseases, said in a prepared statement.
Therein lies one of the major reasons why, as Vicari notes, there is not yet "a consensus whether the vaccine can be useful or not." Haiti's population far exceeds the current manufacturing capacity of 5 million doses combined of Shanchol and Dukoral. To vaccinate the entire country with the required two doses per person, it would either take a five-year effort (with immunity waning in each person after two years) or there would need to be a massive scale-up effort in production. "Regardless of financial issues, that is going to be a little bit of a bottleneck," Vicari says.
As Olson pointed out, a strategic use of the limited quantities of vaccine could be possible: vaccines could first be sent to remote regions, where deliveries of soap, clean water and training are more difficult. "It won't be easy to vaccinate in rural areas with poor access, but it would be even harder to intervene should an outbreak occur," Olson said. But not everyone agrees on an appropriate use of the limited supply. Early on in the epidemic, the then-Haitian health minister even expressed concern that having a limited number of doses could cause unrest.
Partners In Health has eliminated that issue from their program by servicing two areas that each has about 50,000 residents, "so we can vaccinate almost everyone in those areas," Weigel explains, who also notes that unvaccinated individuals in these communities would benefit from herd immunity.
Farmer predicts that if the government decides to support the vaccine's more widespread distribution, supply will follow and thereby render the current debate irrelevant. "There are hundreds of thousands of cases just in Haiti—and millions around the world, so if demand were in any way related to burden of disease," there should be adequate supply, he says.
Excising the endemic
Even if the vaccine demonstration proves successful in Bocozel and Cité de Dieu, the cholera scourge is not going to be rid from Haiti with immunization alone. As Weigel is quick to point out, "it would be foolhardy" to try to eradicate cholera from the area using only a vaccine.
The cholera eradication conversation inevitably turns back to the need for potable water and better sanitation. "Without improving access to clean water and proper sanitation, cholera will undoubtedly keep coming back," Olson said.
And that infrastructure is expensive to build. But as Mirta Roses, director of PAHO, said in a press briefing Wednesday, not improving water and sanitation will be even more costly. "It might take years, but the journey begins today," she said.
At the end of the day, however, the path forward will be for the Hatian government to select and see through. Haitian President Michel Martelly addressed the PAHO briefing, noting that, "the time has come to address these deficiencies," adding that "only a joint, comprehensive and strategic approach can lead us to eliminate cholera."
Martelly, PAHO and others have taken as a model for cholera's eradication the lessons learned from the reemergence of the pathogen in Latin America in the 1990s, which took a decade to vanquish.
But for many Haitians at risk for contracting cholera, 2020 could come too late. Farmer and his colleagues at Partners In Health are hoping that widespread use of the vaccine could bolster other longer-term investments to in the cholera combat. "We do hope that will be a model for Haiti, and the ministry of health has been extremely excited about it," Weigel says of the Partners In Health demonstration.
And like water improvement, the vaccine shakes out to look like a good investment—and one that could draw quicker dividends. The $40 million needed to pay for vaccine doses for the entire country—if they were to be available—seems like just a drop in the bucket of the billions of dollars promised following the disaster two years ago. But as Vicari points out, "what is pledged is not necessarily what is available." So far, "just 30 to 40 percent was received."
Nevertheless, investing in cholera prevention by procuring more vaccines could also cut down on costs in the future, Weigel points out. In the 14 months since the first cholera cases appeared, the disease has cost some $176 million—many times that of the cost of vaccination, he notes. "This is low-hanging fruit—this is not some complex intervention."
This article was first published on Scientific American. © 2011 ScientificAmerican.com. All rights reserved. Follow Scientific American on Twitter @SciAm and @SciamBlogs. Visit ScientificAmerican.com for the latest in science, health and technology news.
La Crosse virus disease: The rare mosquito-borne illness that causes deadly brain inflammation
Parasitic worm raises risk of cervical cancer, study finds