Artificial Testicle Could Treat Male Infertility

Researchers in California hope to become the first in the world to build an artificial testicle that produces human sperm. Such a device could allow infertile men to conceive children.
While recent studies have shown it's possible to treat infertile male mice by producing sperm using stem cells from the mouse, the same has not been done for humans, said researcher Dr. Paul Turek, director of the Turek Clinic, a men's health medical practice in San Francisco.
Using a newly received government grant, Turek and his fellow researchers hope to develop a human "sperm-making biological machine," he said.
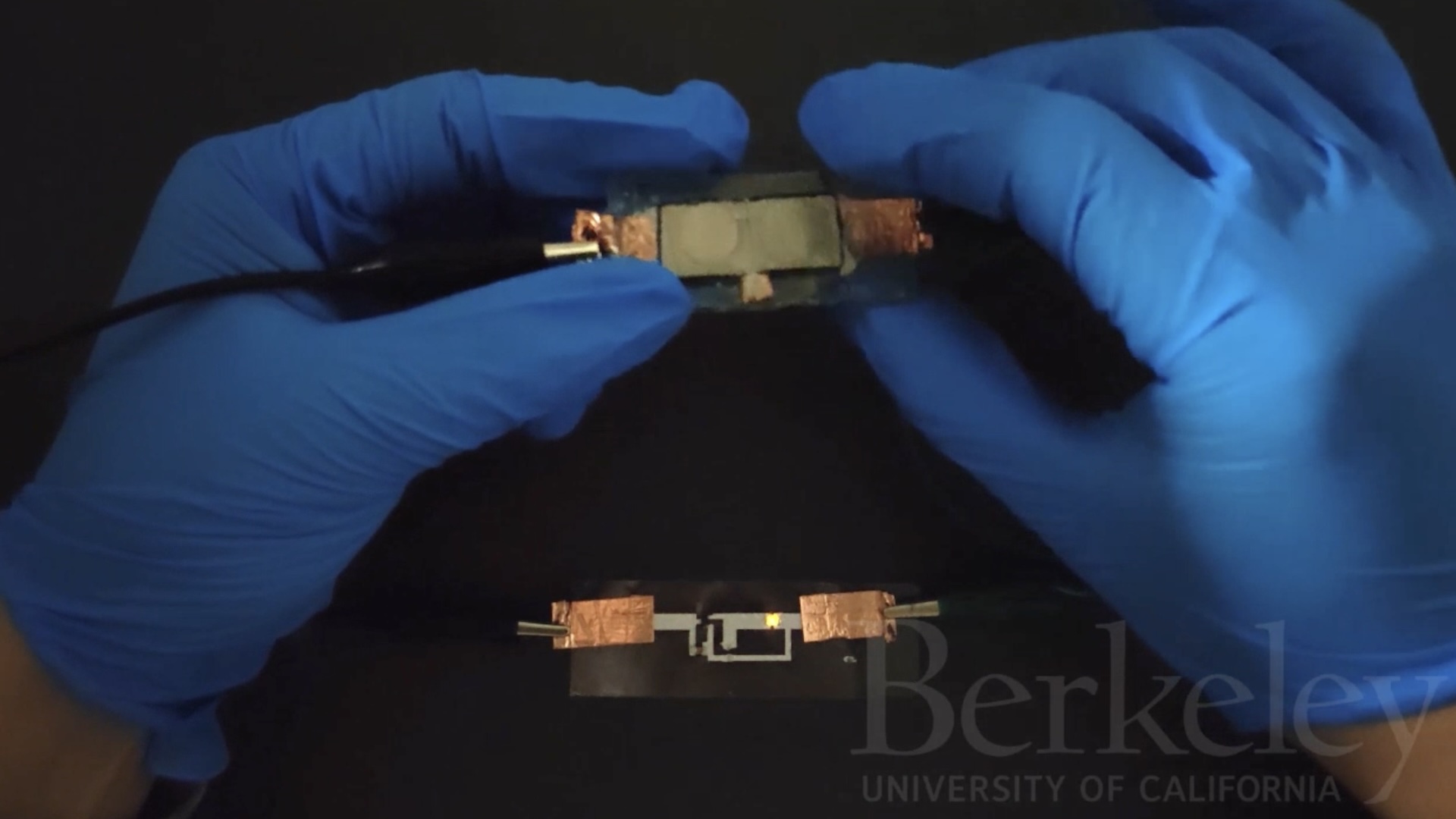
Unlike a non-sperm-producing prosthesis — a saline-filled implant for men missing a testicle — the device will not be designed to resemble a testicle. Instead it will most closely resemble a cylindrical bag a few inches long, Turek said, creating a final product that looks something like a transparent, over-sized Tootsie Roll.
Recreating the testicle
Others have tried to grow sperm from cells in lab dishes, but the cells wouldn't go through all the necessary steps, Turek said. Normally cells in the testicle go through about 12 stages on their way to becoming functioning sperm, but in a dish they stop at stage 9 or 10 — only within the highly specialized environment of the testicle can they complete the process.
Turek said he and his colleagues want to "re-create the testicle in an artificial environment, with all of its components."
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
To make their artificial testicle, the researchers will first focus on growing cells that normally nurture sperm during their development, including cells called Sertoli cells. Then the researchers will add embryonic stem cells, which can turn into virtually any cell in the human body. These stem cells will be "fortified" with genes to steer them down the right path, so that the stem cells develop the properties of sperm precursor cells, Turek told MyHealthNewsDaily.
In essence, the researchers are hoping re-create the environment within the seminiferous tubules, the structures in the testes where sperm are formed.
The artificial testicle would likely last only as long as it takes to go through one cycle of sperm production, about 70 days, Turek said. After that, another one would have to be created.
Ambitious project
"It's an ambitious project," said Kyle Orwig, an associate professor of obstetrics, gynecology and reproductive sciences at the University of Pittsburgh who studies ways to restore male fertility."But it would be fantastic if it happened. It would be a major impact on the fertility field."
No one has yet tried to create sperm by re-creating the "home" of sperm cell production and adding stem cells, Orwig said.
It eventually might be possible to use the model to produce sperm for men who are infertile.
To do this, the researchers probably would use adult stem cells from the patient rather than embryonic stem cells. Such cells could be taken from the patient's skin, and researchers would have to "turn back the clock" so the cells could develop into sperm. But whether this could work remains to be seen, Turek said.
Turek and his colleague Dr. Constance John, chief executive of MandalMed Inc., a biotech company in San Francisco, received a Small Business Innovation Research grant from the National Institute of Environmental Health Sciences. Such grants are typically less than $500,000, Turek said.
Turek hopes to complete the artificial testicle in five to seven years.
Pass it on: Researchers are starting a project to create an artificial human testicle that can produce sperm.
This story was provided by MyHealthNewsDaily, a sister site to LiveScience.Follow MyHealthNewsDaily staff writer Rachael Rettner on Twitter @RachaelRettner. Find us on Facebook.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.
Is getting an IUD painful?
'Useless' female organ discovered over a century ago may actually support ovaries, study finds