Five Myths About Breast Cancer
Cancer experts hope that this October, which is National Breast Cancer Awareness Month, brings more than just awareness about breast cancer but real facts, too.
While pink ribbons are everywhere as a means to raise awareness and show support to cancer patients, a survey commissioned by the National Breast Cancer Coalition reveals that most women know only half-truths about breast cancer, which will claim more than 40,000 lives in 2007.
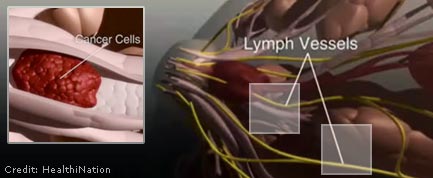
Among the most worrisome misconceptions are that breast cancer is largely hereditary and that it can be prevented.
Myth 1: Risk factors are mostly to blame
The majority of the 1,000-plus women surveyed thought that heredity is the cause of most breast cancers. In reality, only 5 to 10 percent of those diagnosed with breast cancers have a family history. More than two-thirds of women with breast cancer have no known risk factors.
There is a strong genetic component. Women with certain mutations within the BRCA1 and BRCA2 genes have a 60- to 80-percent chance of developing breast cancer. Fortunately, this mutation is rare.
Obesity and alcohol are two other known risk factors, behind about 20 percent of breast cancers. Obesity nearly triples the risk of breast cancer, according to the Women's Health Initiative study of 85,917 postmenopausal women. And consuming four alcoholic drinks a day raises the risk by 1.5 times, according to the National Cancer Institute.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Yet, tragically, most women are developing breast cancer while leading relatively healthy lives.
Myth 2: One in eight women will get it this year
Most women in the survey thought that one in eight women will be diagnosed with cancer this year. Fortunately, no. That "one in eight" number tossed around refers to the lifetime risk of developing breast cancer. Fewer than 200,000 women will be diagnosed this year. With approximately 150 million females in America, that translates to about one in 750 women.
Survival rates are quite good these days, too. The lifetime risk of dying from breast cancer for women is about one in 35, or 3 percent, according to the American Cancer Society.
Not to minimize breast cancer, but the greater cancer scourge—and utterly preventable—is lung cancer from cigarette smoking, constituting about a quarter of all cancer deaths and nearly 70,000 U.S. female deaths yearly. [Men can get breast cancer , too.]
Myth 3: Breast cancer is preventable
Most women surveyed thought that breast cancer can be prevented, particularly by eating fruits and vegetables. But when the biggest risk factors are being female and getting older, there's not much a woman can do. You can reduce but not eliminate the risk.
Studies have not shown convincingly that fruits and vegetables ward off breast cancer. However, the Women's Intervention Nutrition Study and other studies have revealed that lowering dietary animal fat lowers the risk of breast cancer, consistent with the notion that breast cancer rates are highest in regions with meat-heavy "Western" diets.
Myth 4: Self-examination is the solution
Early detection and treatment is key for breast cancer survival. Yet most survey respondents placed too much faith in self-examinations and mammograms . Mammograms are among the best diagnostic tools we have, but they are imperfect, revealing too many false positives and thus leading to worry and to unnecessary procedures. Mammograms also miss a surprising number of real, malignant cancers.
Similarly, self-examinations can be useful if done properly, but they do not reduce deaths due to breast cancer and they greatly increase the number of benign lumps detected, resulting in increased anxiety and unnecessary biopsies.
Myth 5: Abortions cause breast cancer
A persistent myth that the survey did not address is that abortions can cause breast cancer. This is based on real science—studies of rats in the 1980s indicating a possible correlation between hormones and breast tissue growth. But the issue was thoroughly resolved by the 1990s.
Nevertheless, the Bush Administration revisited the issue in 2002, gave equal weight to the earlier, smaller studies showing a correlation, and told the National Cancer Institute to state the possible abortion-cancer connection in its fact sheets and Web site. It took Congressional action and a three-day conference on the topic to remove this erroneous information by 2003.
- Phony Cancer Scares Debunked
- Exciting New Cancer Treatments Emerge Amid Persistent Myths
- Top 10 Mysterious Diseases
Christopher Wanjek is the author of the books “Bad Medicine” and “Food At Work.” Got a question about Bad Medicine? Email Wanjek. If it’s really bad, he just might answer it in a future column. Bad Medicine appears each Tuesday on LiveScience.

Christopher Wanjek is a Live Science contributor and a health and science writer. He is the author of three science books: Spacefarers (2020), Food at Work (2005) and Bad Medicine (2003). His "Food at Work" book and project, concerning workers' health, safety and productivity, was commissioned by the U.N.'s International Labor Organization. For Live Science, Christopher covers public health, nutrition and biology, and he has written extensively for The Washington Post and Sky & Telescope among others, as well as for the NASA Goddard Space Flight Center, where he was a senior writer. Christopher holds a Master of Health degree from Harvard School of Public Health and a degree in journalism from Temple University.