Some Fungal Meningitis Patients Slowly Recovering
The therapies used to treat patients affected by the fungal meningitis outbreak appear to be working, and some may be on the road to recovery, medical experts say.
At one hospital, the Carilion Clinic -Roanoke Memorial Hospital in Virginia, most patients with fungal meningitis who were treated with the antifungal medication voriconazole are improving, albeit slowly, said Dr. Anthony Baffoe-Bonnie, an infectious disease specialist at the Virginia Tech Carilion School of Medicine. In fact, eight of his 25 meningitis patients improved enough to go home after about three weeks of treatment, Baffoe-Bonnie said.
Patients were allowed to go home if their symptoms, which included severe headache, had diminished, and they tolerated the antifungal treatment well, Baffoe-Bonnie said. In addition, the number of white blood cells in their cerebral spinal fluid — a measurement that typically indicates infection — needed to drop, he said. [See Meningitis Outbreak: Should Anti-Fungal Meds Be Given to Those at Risk?].
Some patients experienced problems in their ability to recall words, but this did not seem to affect their overall quality of life, Baffoe-Bonnie said.
However, it's too soon to say these patients are cured, and it's always possible some may have their condition worsen, Baffoe-Bonnie said. Patients who've been released still come back to the clinic for regular checkups, and have their cerebral spinal fluid checked about once a month.
As of Friday (Nov. 9), 438 people nationwide have been affected by the outbreak, including 32 who have died. Most patients became infected after receiving contaminated steroid injections in the spine.
Before the outbreak of fungal meningitis was reported in late September, cases of this particular type of meningitis had been rare, and little information existed regarding what patients and doctors could expect from treatment. To fill this information gap and potentially guide future treatments, Baffoe-Bonnie and colleagues reported the early results of treating patients at their hospital. Their report was published online yesterday (Nov. 12) in the journal Annals of Internal Medicine.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
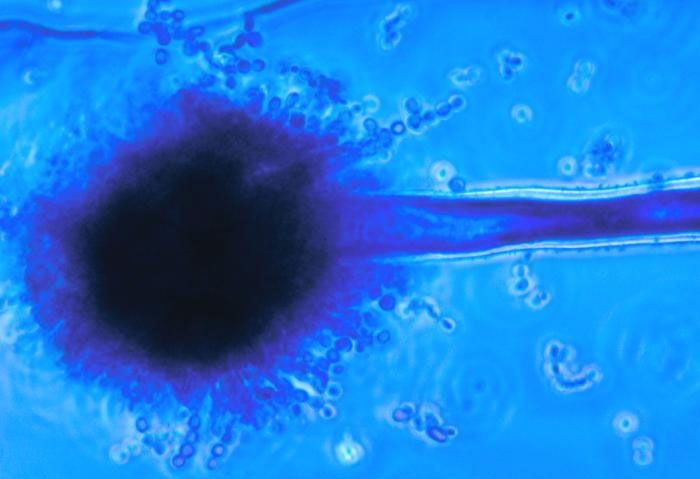
A total of 172 patients visited the hospital's emergency department between Oct. 4 and Oct. 31 believing they may have been infected with meningitis. Of these, 131 underwent a lumbar puncture (spinal tap) to examine their cerebral spinal fluid. Of these, 25 were diagnosed with fungal meningitis, and eight were confirmed to be infected with the fungus Exserohilum.
All patients had severe headaches they described as the "worst they had ever had."
The white blood cell count in the patients' cerebral spinal fluid began to decrease, on average, after 13 days of treatment, the researchers said. Fifteen patients continued to be treated with voriconazole, but 10 were switched to the drug amphotericin-B due to worsening symptoms or the side effects of voriconazole, which include hallucinations.
A few patients in the hospital have recovered enough that their main complaint is boredom as they wait for their spinal fluid measurements to improve, the researchers said.
But others continue to experience symptoms, including arachnoiditis, a painful inflammation of one of the membranes that surrounds the spinal cord. The condition can cause numbness, tingling and burning pain in the lower backs and legs.
It's not clear how long patients will need to receive treatment and have checkups, but it's likely to be a prolonged period, Baffoe-Bonnie said.
Pass it on: Antifungal treatments given to patients affected by the meningitis outbreak appear to be working, albeit slowly.
Follow Rachael Rettner on Twitter @RachaelRettner, or MyHealthNewsDaily @MyHealth_MHND. We're also on Facebook & Google+.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.