Scientists Discover New Mechanism for Antibiotic Resistance
One of the greatest threats to public health in the Third World is strains of tuberculosis bacteria that have grown resistant to antibiotics and other traditional medicines.
Now, scientists in Japan and Switzerland have witnessed a previously unknown method a certain bacterium uses to evade the best weapons in the medical armory. The discovery, made in a bacterium similar to the one that causes TB, could potentially lead to more effective drugs.
Reported in the latest issue of the journal Science, the finding also casts doubt on the conventional explanation of how bacteria develop resistance to drugs.
Making drugs that are more effective against tuberculosis is not a minor matter. According to the World Health Organization, there are parts of the world where one-quarter of all TB patients have a drug-resistant form of the disease, called multidrug-resistant tuberculosis, or MDR-TB. WHO reports that 440,000 people had MDR-TB in 2008 worldwide and a third of them did not survive. Half the cases are in India and China. There is an extreme version, XDR-TB, that is even worse.
MDR-TB is less of a problem in the developed world but treatment is still difficult and expensive.
Most antibiotics attack bacteria cells as they divide, preventing them from building cell walls. A widely held theory of antibiotic resistance is that bacteria contain some cells that do not divide, called persister cells. Since they don’t divide, they are not affected by drugs that attack cell division. The persister cells remained stubbornly unaffected.
The researchers, at the University of Tokyo and the Swiss Federal Institute of Technology in Lausanne, think this is not what is happening.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
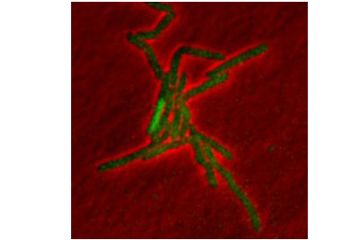
Using a cousin of TB bacterium called Mycobacterium smegmatis often used in laboratories because it is safer than using an actual TB bacterium, they tested a front-line TB medicine called isoniazid. Working in a lab in Switzerland, they found an entirely different mechanism involved in the persistence.
Isoniazid is a “pro-drug,” which means it doesn’t do anything until it interacts with chemicals in the bacterial cell. When the drug meets an enzyme produced by the cell known as KatG, isoniazid gets switched on.
Persistence had nothing to do with cell division or the growth rates of the cell, the researchers found. The cells produced KatG in random pulses. The drug did not work between pulses, and the cells that were not producing KatG survived.
“Pulsing is an infrequent and short-lived phenomenon, and most cells go from birth to next division without pulsing,” said the Swiss institute's John McKinney, one of the lead authors.
Presumably, if the drug were present long enough, it would catch all the cells undergoing a pulse of KatG and end the infection.
“But remember, one of the unexpected findings in our study is that [persister] cells continue to grow and divide in the presence of antibiotics, which continuously replenishes the population,” McKinney said. Those cells that survive would mutate resistance, he said.
So far, McKinney said, the team has not found a pattern in the pulsing. It appears entirely random.
The current treatment for non-resistant TB is a regimen of four antibiotics taken daily for four to six months, according to David Dowdy, assistant professor at the Johns Hopkins Bloomberg School of Public Health. The treatment is expensive because nurses have to make sure the patient takes the medication regularly, either with a home or office visit.
The treatment for resistant tuberculosis “is longer, expensive and more toxic,” Dowdy said. It can last 21 months and require a daily injection for the first six to eight months.
“Many people can’t tolerate it,” Dowdy said. “Not only are the drugs unpleasant but [they] have important toxicities.”
The cure rate for non-resistant TB is about 90 percent, he said. The cure rate for people with resistant TB--if they take their medicine--is around 70 percent.
Whether the same mechanism the Swiss-Japanese team found is working with other kinds of bacteria is impossible to say yet, McKinney said,
“I would not hazard a guess,” McKinney said. “For a long time, the persistence field has been held back by over-extrapolating the results from one system to other systems and I would rather not contribute to the muddle.”
Dowdy said the research is useful to know because it might help improve the cocktail of antibiotics TB patients need to take.
The problem, he said, is that there are so few alternatives to the antibiotics now available.
“In the future, we might be able to make better decisions,” Dowdy said.
Joel Shurkin is a freelance writer based in Baltimore. He is the author of nine books on science and the history of science, and has taught science journalism at Stanford University, UC Santa Cruz and the University of Alaska Fairbanks.
Inside Science News Service is supported by the American Institute of Physics.












