Hollywood Ending for Christina Applegate's Breast Cancer?
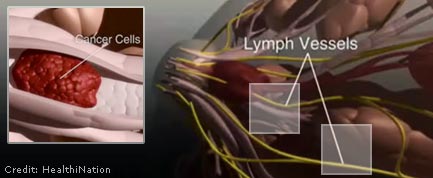
Actress Christina Applegate made a brave decision a few months ago to have a double mastectomy after doctors found cancer in one of her breasts. Her mother had had breast and ovarian cancer, and Applegate carries the BRCA1 gene, making her highly susceptible to these cancers.
This prophylactic mastectomy reduces her cancer risk from about 50 percent to 5 percent. The specter of cancer remains, however, because even the best surgeons have difficulty discerning breast tissue from fat and inevitably will leave behind some breast cells, possibly cancerous.
Applegate's decision to have her breasts removed is all the more remarkable because she is young and in a business so often defined by breasts.
Now she is planning to have breast reconstruction surgery and remains incredibly upbeat. "I'm going to have the best boobs in the nursing home," she told reporter Robin Roberts, herself a cancer survivor, during an interview on ABC's Good Morning America.
This is an inspiring remark, warranting a "You go, girl" reply. Indeed, on the blogsphere, many women seem awed by Applegate's courage and candor.
Applegate's comment, however, is slightly misleading. Reconstruction surgery is not straightforward. Some women who have had mastectomies opt not to have the follow-up surgery. Money is not necessarily the issue; by law the surgery is covered by health insurance. Rather, some women find the risks and process not worth it, particularly when battle-weary from the cancer itself.
Pair of surgical techniques
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
There are two main types of breast reconstruction surgery. The tissue-flap technique uses muscle, fat and skin from other parts of the body. This is major surgery, far more complicated than the mastectomy, often requiring more than a year for recovery.
The price is significant lost muscle strength where the tissue was removed, usually the abdomen. The plus is that the patient is left with a permanent structure — a breast-like sac, actually, with little sensation — that closely resembles the form of a breast when the woman is fully clothed. Some women have the stamina to later add a tattooed areola around an artificial nipple.
The other surgery is a breast implant, but not like implants many women have for reasons of pure vanity. Because one or both breasts have been removed, the surgeon is starting from nothing and must stretch the skin slowly with inflatable implants over the course of many months. The implants bring well-known risks of infection, breakage and slippage and need to be replaced about every ten years or so to maintain their form.
Applegate is likely too thin for the tissue-flap procedure. She has little tissue to spare, and she needs two breasts. For her to have perky breasts at age 90, as she joked, she'd have to have an implant put in around age 90, unlikely given the risk of surgery on someone so old.
National discussion on breasts, the organs
Applegate's candor allows for a discussion of many misconceptions, precisely what so many women facing breast cancer need. Other issues in this story are the cancer gene, the alarming rate of prophylactic mastectomies, and freedom of choice.
Applegate carries the BRCA1 gene, increasing her risk of breast and ovarian cancer by as much as 60 percent, factoring in family cancer history. How great to know you carry this gene, for you could — as Applegate has done — undergo intensive and regular screening for signs of a tumor.
Knowledge comes at a price. Gene tests cost thousands of dollars and typically aren't covered by insurance, placing it out of reach for most Americans. Conversely, while the BRCA1 gene often spells cancer, about 90 percent of women with breast cancer don't have this gene.
Meanwhile, the rate of prophylactic mastectomies has more than doubled since 1998, from 1.8 percent of breast cancer patients to 4.5 percent, according to an article published in the November 2007 issue of the Journal of Clinical Oncology. The numbers are in, but the reason is unknown.
Is the medical establishment pushing for aggressive surgery? There is intelligent discussion on both sides.
Sadly, many women don't have choices. As with gene screening, thorough breast cancer screening with MRI is expensive. Some women — if examined and if diagnosed properly, both far less common than should be expected — are offered poor choices by bad doctors on a procedure, be it radiation, chemotherapy, lumpectomy, various types of mastectomies and reconstruction.
Applegate's story might have a Hollywood ending. This is wonderful. Women need to know, however, that this is her story and that the decisions they make about how to treat breast cancer need not mirror Applegate's to lead to a happy ending.
- 5 Myths About Breast Cancer
- The Top 10 Worst Hereditary Conditions
- Breast Implants Linked to Higher Suicide Rate
Christopher Wanjek is the author of the books "Bad Medicine" and "Food At Work." Got a question about Bad Medicine? Email Wanjek. If it’s really bad, he just might answer it in a future column. Bad Medicine appears each Tuesday on LiveScience.

Christopher Wanjek is a Live Science contributor and a health and science writer. He is the author of three science books: Spacefarers (2020), Food at Work (2005) and Bad Medicine (2003). His "Food at Work" book and project, concerning workers' health, safety and productivity, was commissioned by the U.N.'s International Labor Organization. For Live Science, Christopher covers public health, nutrition and biology, and he has written extensively for The Washington Post and Sky & Telescope among others, as well as for the NASA Goddard Space Flight Center, where he was a senior writer. Christopher holds a Master of Health degree from Harvard School of Public Health and a degree in journalism from Temple University.










