Why do we have different blood types?
Why are some people O+ and others B-?
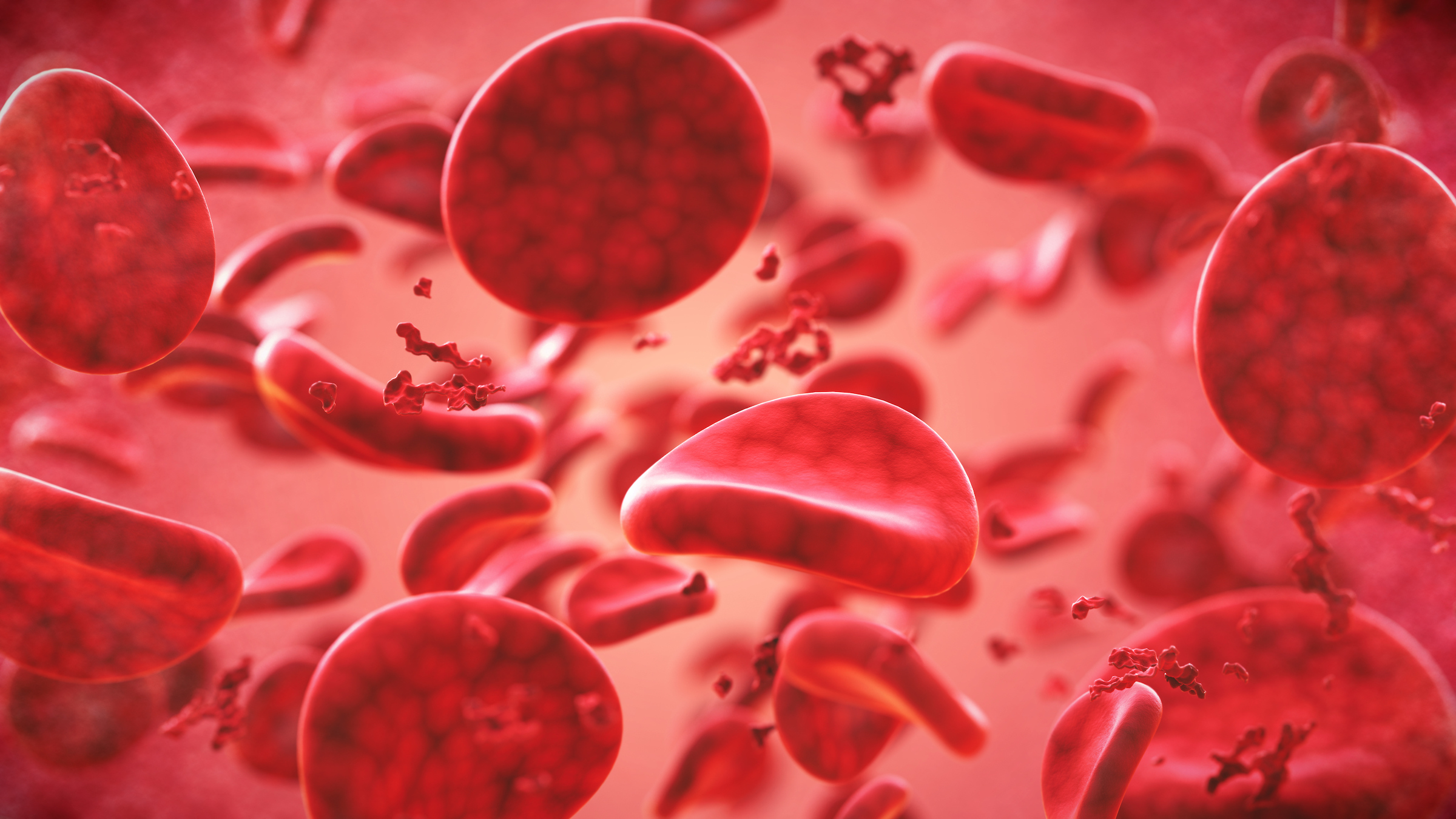
The type of blood coursing through your veins is likely different from the blood in your friends and maybe even your family. Knowing your blood type is important for blood transfusions and other medical purposes, which raises a question: Why do humans have different blood types?
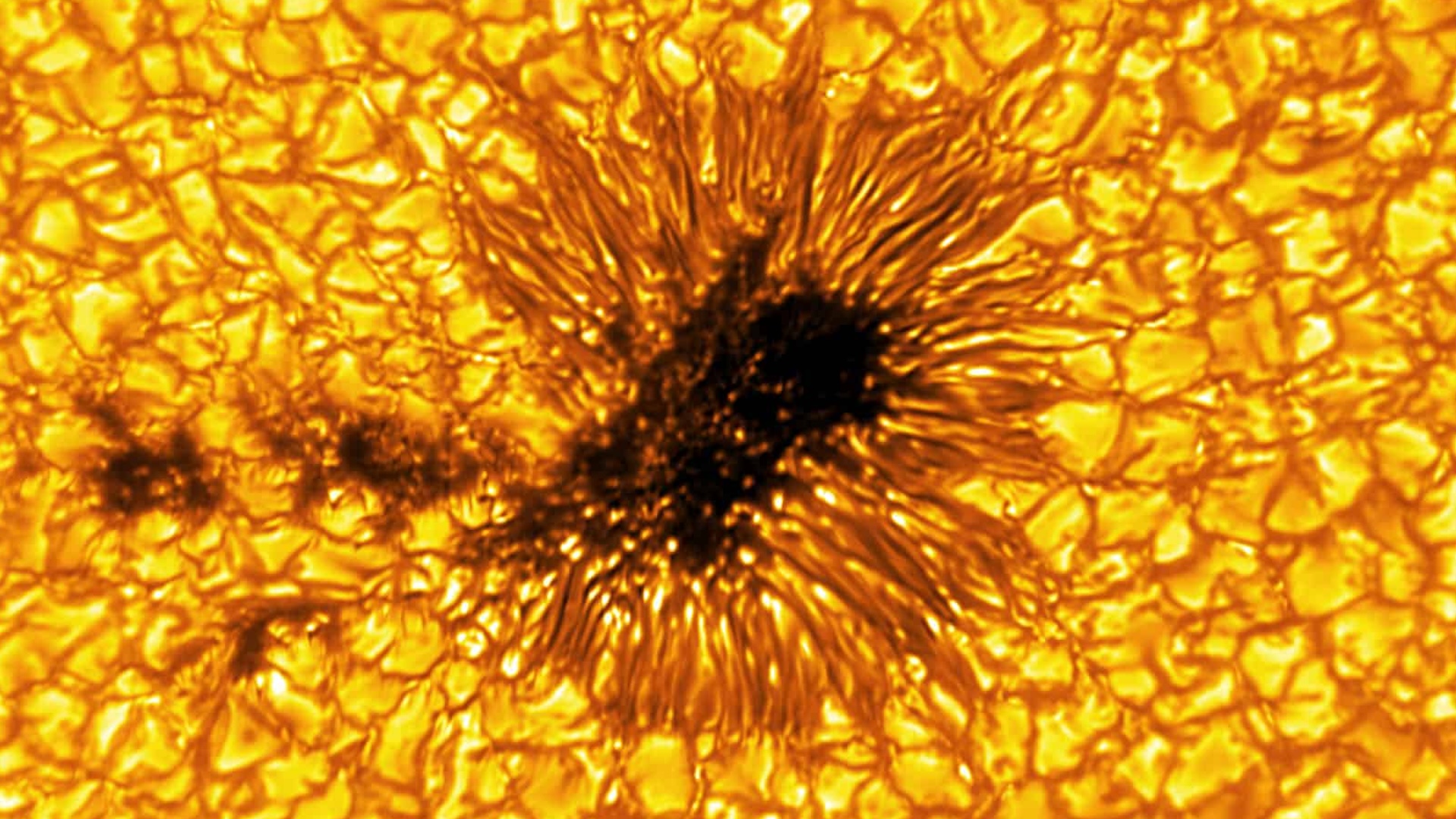
There are four main blood groups: A, B, AB and O. Each is defined by which antigens are present on the surface of red blood cells. Type A blood has the A antigen on red blood cells, B has the B antigen, AB has both and O has neither.
"The data are strongly suggestive that the whole reason we have different blood groups is malaria," said Dr. Claudia Cohn, medical director of the University of Minnesota's blood bank. "If you superimpose a map of where the malaria parasite is and the group O blood type, it is remarkably similar."
Malaria has a high death toll, having killed 627,000 people worldwide in 2020, according to the Centers for Disease Control and Prevention. In people carrying the parasite that causes malaria, infected red blood cells pile up in small blood vessels, blocking blood and the oxygen it carries from getting to the brain. But people with group O blood have significant protection against malaria. A 2007 study in the journal Proceedings of the National Academy of Sciences, for example, found that people with type O blood were 66% less likely to develop severe malaria than people with other blood types.
Related: What's the rarest blood type?
This is at least partially because the malaria parasite makes infected red blood cells express a protein on their surface called RIFIN, which acts like a glue that makes uninfected red blood cells pile up around an infected red blood cell, according to a 2015 study in the journal Nature Reviews Microbiology. But whereas RIFIN binds strongly to the surface of type A red blood cells, it binds weakly to type O red blood cells, according to a 2015 study in the journal Nature Medicine.
Yet blood group isn't the only aspect of a person's blood that affects their malaria risk. In addition to those that cause the four main blood groups, there are 15 other types of antigens that can be present on the surface of red blood cells, Cohn told Live Science. One of those is called the Duffy group. People who lack the Duffy antigen are relatively resistant to one of the two major malaria parasites. Duffy negativity is common throughout sub-Saharan Africa, where malaria is most prominent, but it is rarely seen elsewhere in the world, according to the Malaria Atlas Project.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
There's quite a bit of evidence for why populations that evolved in malaria-prone areas have type O blood, but it's less clear why type A, B and AB blood can be found in relatively high proportions elsewhere. Some scientists point to disease associations between various blood types. For example, a 2021 study in the journal BioMed Research International found that people with type O blood are more likely to have cholera, plague, tuberculosis and mumps. Other blood types are more likely to have other diseases; for example, people with type AB blood are more likely to have smallpox and Salmonella and E. coli infections.
Cohn doesn't find these associations convincing, though, especially not as a potential reason for why humans have different blood types. These studies did not prove a causal relationship between blood type and the prevalence of these diseases; the links may be due to other factors. As such, they don't actually find evidence of blood types causing protection or susceptibility to diseases. "Malaria is the only one where it really seems to bear itself out," she said.
It's also unclear why most people have a protein known as the Rhesus (Rh) factor on the surface of their blood cells, making them Rh positive, although about 15% of Caucasians, 8% of Black people, and 1% of Asians lack this protein, making them Rh negative. (This is what the + and - that follow blood groups indicate, for example A+ or B-.) In a 2012 study published in the journal Human Genetics, researchers investigated whether there was an advantage to being Rh negative that would keep this genetic variation around, despite it sometimes causing rhesus disease — a condition in which a pregnant person's antibodies attack their baby's blood cells. However, they couldn't find one, so they concluded that either the benefit existed in the evolutionary past and does not anymore, or humans have those two Rh types because of random chance.
Originally posted on Live Science on Sept. 29, 2011 and rewritten on March 28, 2022.

Tyler Santora is a freelance science and health journalist based out of Colorado. They write for publications such as Scientific American, Nature Medicine, Medscape, Undark, Popular Science, Audubon magazine, and many more. Previously, Tyler was the health and science Editor for Fatherly. They graduated from Oberlin College with a bachelor's degree in biology and New York University with a master's in science journalism.