Chronic fatigue syndrome: Causes, symptoms and treatment
Chronic fatigue syndrome is a complex, multisystem disease that can often go undiagnosed.

Chronic fatigue syndrome (CFS), also known as myalgic encephalomyelitis (ME), is a serious, long-term illness that affects many body systems. People with chronic fatigue syndrome are often not able to go about their usual activities due to severe fatigue and sleep problems. Other symptoms can include problems with thinking and concentrating, pain and dizziness. At least one-quarter of CFS patients are bed- or house-bound for long periods during their illness, according to the Centers for Disease Control and Prevention (CDC).
An estimated 836,000 to 2.5 million Americans may suffer from chronic fatigue syndrome, according to an Institute of Medicine report. However, up to 90% of them may not have been diagnosed.
Dr. Adam Staten, a general practitioner and clinical director at One Day Tests, a blood testing company in England, told Live Science that it is unclear what causes CFS.
"Chronic fatigue syndrome is an enigmatic and intensely frustrating condition," he said. "Despite being fairly common, [it] remains poorly understood. But research teams around the world are slowly beginning to shed light on its causes."
What are the symptoms of chronic fatigue syndrome?
According to the CDC, all three primary ("core") symptoms and at least one secondary symptom are required for a diagnosis of CFS. There are many other symptoms that may present with the condition, but they are not essential for a diagnosis.
Primary symptoms
- Severe fatigue and a substantial drop in activity level (lasting six months or longer): The fatigue is not a result of unusually difficult activity, is not relieved by sleep or rest, and was not a problem before becoming ill.
- Post-exertional malaise (the worsening of symptoms after physical or mental activity that would not have caused a problem before illness): During post-exertional malaise, any ME/CFS symptoms may get worse or first appear. It may take days, weeks, or longer to recover from a relapse.
- Sleep problems: Patients may not feel better or less tired, even after a full night of sleep. Some people with CFS may have problems falling asleep or staying asleep.
Secondary symptoms
- Problems with thinking and memory: Trouble thinking quickly and or clearly, memory problems and poor attention to details.
- Orthostatic intolerance (worsening of symptoms while standing or sitting upright): Feeling lightheaded, dizzy, weak, or faint while standing or sitting up.

Other common symptoms of CFS, according to the CDC, include:
- Pain (usually muscle pain and aches, joint pain without swelling or redness, and headaches)
- Tender lymph nodes in the neck or armpits
- A sore throat that happens often
- Digestive issues, like irritable bowel syndrome
- Chills and night sweats
- Allergies and sensitivities to foods, odors, chemicals, light, or noise
- Muscle weakness
- Shortness of breath
- Irregular heartbeat
Chronic fatigue syndrome is most common in people age 40 to 60. Women are affected more than men, however, anyone can develop this condition, the CDC says.
What causes chronic fatigue syndrome?
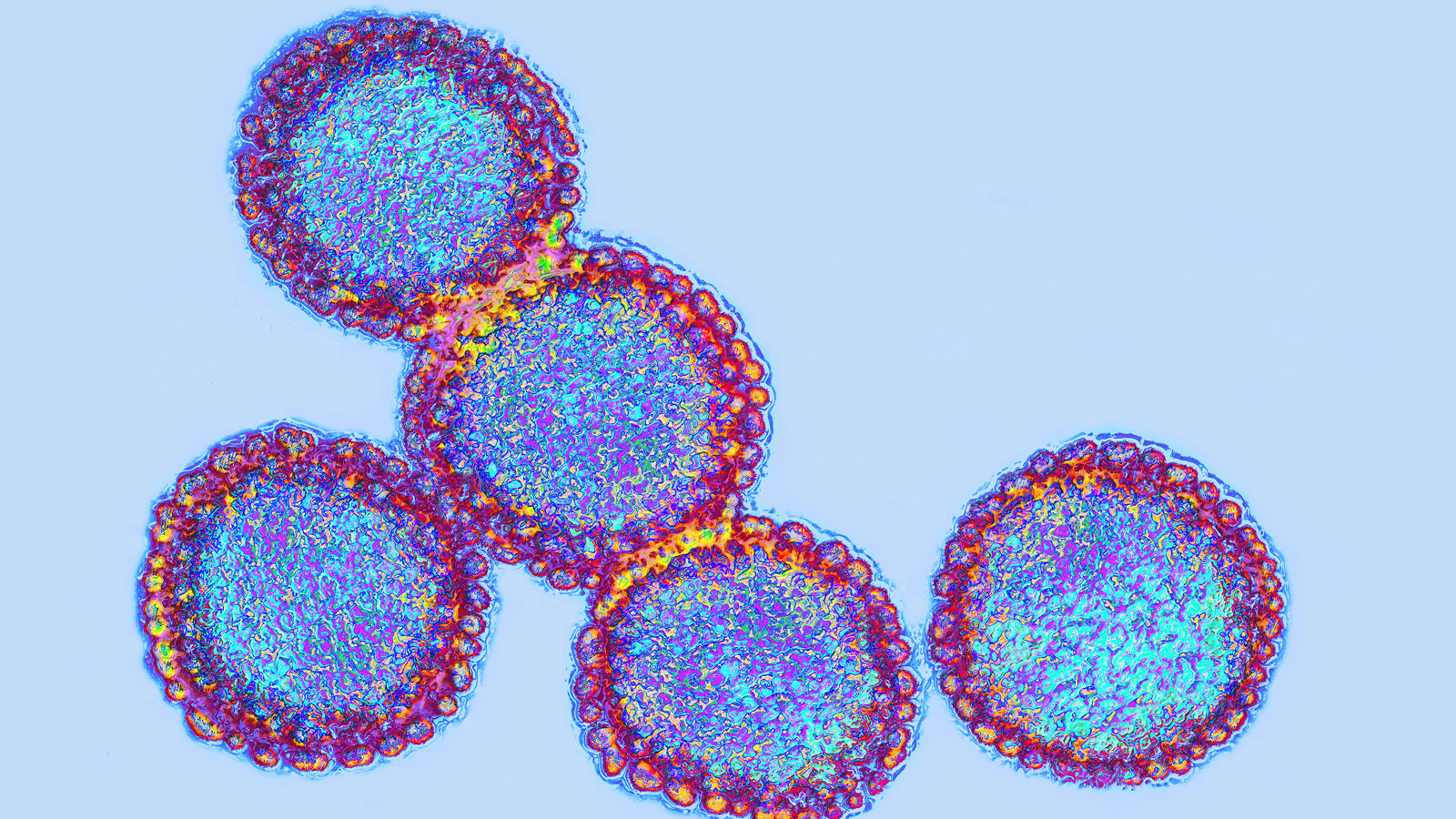
According to the CDC, it is unclear what causes chronic fatigue syndrome. Scientists suggest that it may have more than one cause. Some of the areas that are being studied include infection, immune system dysregulation (when the body cannot control or sustain an immune response), stress and genetic factors. It's possible that two or more triggers might work together.
"It may be that the condition we know as CFS will eventually be shown to be a number of different conditions with similar symptoms, each of which may need different treatment strategies," Staten said.
Infections
Chronic viral infection as a cause of CFS has long been debated, Staten said.
"As far back as the early 80s, some studies demonstrated the link between infection with the Epstein Barr virus [which causes mono] and prolonged symptoms of malaise and fatigue," he said. "There has long been a suspicion that infections, and the immune response to those infections, may play a role in the development of CFS."
However, no link between CFS and infectious agents has been confirmed, and the role of viral and bacterial infections in this condition remains unclear, according to a 2018 review published in the Journal of Translational Medicine.
Immune system dysregulation
There is convincing evidence that some cases of CFS may be caused by excessive autoimmune responses, according to a 2018 review published in the journal Autoimmunity Reviews.
"Researchers have been able to demonstrate that certain autoantibodies are more common in sufferers of ME/CFS, which has fuelled speculation that CFS may be an autoimmune condition which, like other autoimmune conditions, may be triggered by infection," Staten said.
Cardiovascular
According to a 2021 review in the Journal of the American College of Cardiology, patients with CFS often have abnormalities in the cardiovascular system, such as reduced stroke volume (volume of blood pumped by the heart). Low oxygen consumption in the lungs may be another key feature of CFS, according to a 2019 review published in the International Journal of Sports Medicine.
Cardiovascular abnormalities could explain why many people with CFS can experience symptoms such as dizziness on standing and palpitations, Staten said. However, more evidence is needed to understand this association.
"Whether these cardiovascular abnormalities are truly related to ME/CFS, and whether they are a cause of the condition or a result of it, still needs more research," Staten said. "It does suggest a potential target for treatment."
Genetics
Studies have shown that 199 genetic alterations spread across 14 different genes were present in 91% of cases in the CFS population, according to a 2022 review published in the Journal of Translational Medicine. Many of these genes play a key role in regulating mechanisms that may underpin CFS, such as vulnerability to infection and impaired energy metabolism, the review researchers said.
Brain
MRI studies have shown structural changes in the white and gray matter in the brain of CFS patients, according to a 2021 review published in the journal Frontiers in Neurology. Scientists have also found abnormalities in the connectivity between different parts of the brain.
Patients with CFS also tend to have impaired blood flow in the brain and increased intracranial pressure (pressure within the skull), according to a 2021 review published in the Journal of Translational Medicine. Researchers suggested that these mechanisms may explain certain symptoms of CFS, such as brain fog, cognitive impairment, sleep problems and headaches.
How is chronic fatigue syndrome diagnosed?
Chronic fatigue syndrome is only diagnosed after ruling out all other reasons for symptoms. To do that, a doctor will ask about the medical history of the patient and their family, perform physical and mental status examinations, and order blood, urine or other tests. Patients may also be asked to keep an activity journal, according to the CDC.
A number of factors complicate diagnosis, including the fact that there is no laboratory test or biomarker for CFS. Fatigue and many other symptoms resemble those associated with a range of illnesses, further complicating diagnosis. The condition is characterized by periods of remission and relapse, which means that patients who have the syndrome may not always appear to be suffering from it. Because symptoms vary widely, it may be difficult for medical professionals to identify cases of CFS.
How is chronic fatigue syndrome treated?
There is no cure or known medication for chronic fatigue syndrome. However, some symptoms can be managed, according to the CDC. Patients, their families and healthcare providers should work together to decide which symptom causes the most problems and treat this first. They should discuss the possible benefits and harms of any treatment plans, including medicines and other therapies, the CDC says. Patients are usually treated by multidisciplinary teams, due to the complexity of their condition.
Supporting patients' mental health is one of the keys to managing their symptoms, said Catherine Tregoning, a chartered health psychologist and mental health officer at U.K.-based Autoimmune and Support Awareness Foundation, a nonprofit aimed at improving awareness and reducing the isolation of those with autoimmune conditions.
"Whilst recent research clearly demonstrates ME/CFS is not a psychological condition, it may be triggered by weakening of the immune system following stress or trauma," she told Live Science in an email.

Stress, anxiety and depression resulting from coping with a chronic disorder can exacerbate the physical symptoms of ME/CFS, Tregoning said. Current recommendations from the U.K.'s National Institute for Health and Care Excellence (NICE) support that alongside medical treatment, patients are helped psychologically, socially, emotionally and practically to maintain independence and mobility.
A significant number of studies support the use of cognitive behavioral therapy (CBT) and graded exercise therapy (GET) as treatments for patients with CFS. However, criticism on the scientific rigor of these studies has been raised, according to a 2020 review published in the Journal of Health Psychology.
Many health bodies, including NICE, have stopped recommending CBT and GET as a result. Instead, NICE recommends that patients with CFS should be encouraged to remain within their "energy envelope" — maintaining their expended energy at a level consistent with their available energy — so as not to worsen symptoms. The guidance also promotes the use of psychological therapy as a complementary treatment.
This article is for informational purposes only, and is not meant to offer medical advice.
Additional resources
- Find out more about the symptoms and causes at the Mayo Clinic.
- The Solve ME/CFS Initiative (Solve M.E.) has advice and support.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.

Anna Gora is a health writer at Live Science, having previously worked across Coach, Fit&Well, T3, TechRadar and Tom's Guide. She is a certified personal trainer, nutritionist and health coach with nearly 10 years of professional experience. Anna holds a Bachelor's degree in Nutrition from the Warsaw University of Life Sciences, a Master’s degree in Nutrition, Physical Activity & Public Health from the University of Bristol, as well as various health coaching certificates. She is passionate about empowering people to live a healthy lifestyle and promoting the benefits of a plant-based diet.