Lactose intolerance: causes, symptoms & treatments
Suspect you're suffering from lactose intolerance? Find out more in our complete guide to the condition

If you keep getting bloated, gassy and uncomfortable every time you eat dairy products, it’s likely that you may be suffering from lactose intolerance. Lactose is a sugar that is naturally found in cow’s milk and dairy foods like cheese, yogurt and ice-cream. When your body is unable to break it down, it passes to the colon. Undigested lactose aggravates your intestines, causing a host of unpleasant symptoms and significantly affecting your quality of life.
Many people struggle with lactose intolerance. It’s been suggested that up to 68% of the world’s population has some form of lactose malabsorption, including nearly a third of American adults. Yet many don’t know exactly what’s causing this issue, how it presents itself, and how to manage it effectively.
If you suspect you may be lactose-intolerant, but you’re unsure of what to do next, you’re in the right place. Here, we’ve created a complete guide to lactose intolerance to help you understand why you struggle with digesting dairy and what treatment options may be best for you.
What is lactose intolerance?
According to the National Institute of Diabetes and Digestive and Kidney Diseases, lactose intolerance is a chronic condition in which you experience unpleasant digestive symptoms after you consume foods or drinks that contain lactose. Lactose is a sugar that is naturally found in cow’s milk and dairy products, like cheese, yogurts or ice cream. Because it’s a disaccharide – a molecule composed of two other sugars, glucose and galactose – it can’t be absorbed in the body in its primary form. When lactose passes to the colon undigested, it aggravates your intestines, causing unpleasant symptoms.
It’s important to make a distinction between lactose malabsorption and lactose intolerance. Not everyone struggling with digesting lactose will experience the symptoms. To be clinically diagnosed as lactose-intolerant, you have to continuously experience disruptive digestive symptoms.
Lactose intolerance is also different to a milk allergy, which is an immune system disorder. A milk allergy can cause a life-threatening allergic reaction to the proteins found in dairy milk and often appears in infancy, whereas lactose intolerance typically appears later in life and doesn’t pose a risk to life.
Lactose intolerance affects people differently. Some individuals can tolerate much higher amounts of dairy sugar before having any symptoms. Certain ethnic and racial groups are more likely to be at risk too. In the United States, African Americans, American Indians, Asian Americans and Hispanics tend to have higher rates of lactose malabsorption.
Lactose intolerance: Symptoms and causes
According to the National Institute of Diabetes and Digestive and Kidney Diseases, common symptoms of lactose intolerance include bloating, diarrhea, excessive gas, nausea, pain in the abdomen, and vomiting. The severity of these symptoms changes, depending on the amount of lactose ingested and the state of one’s health.
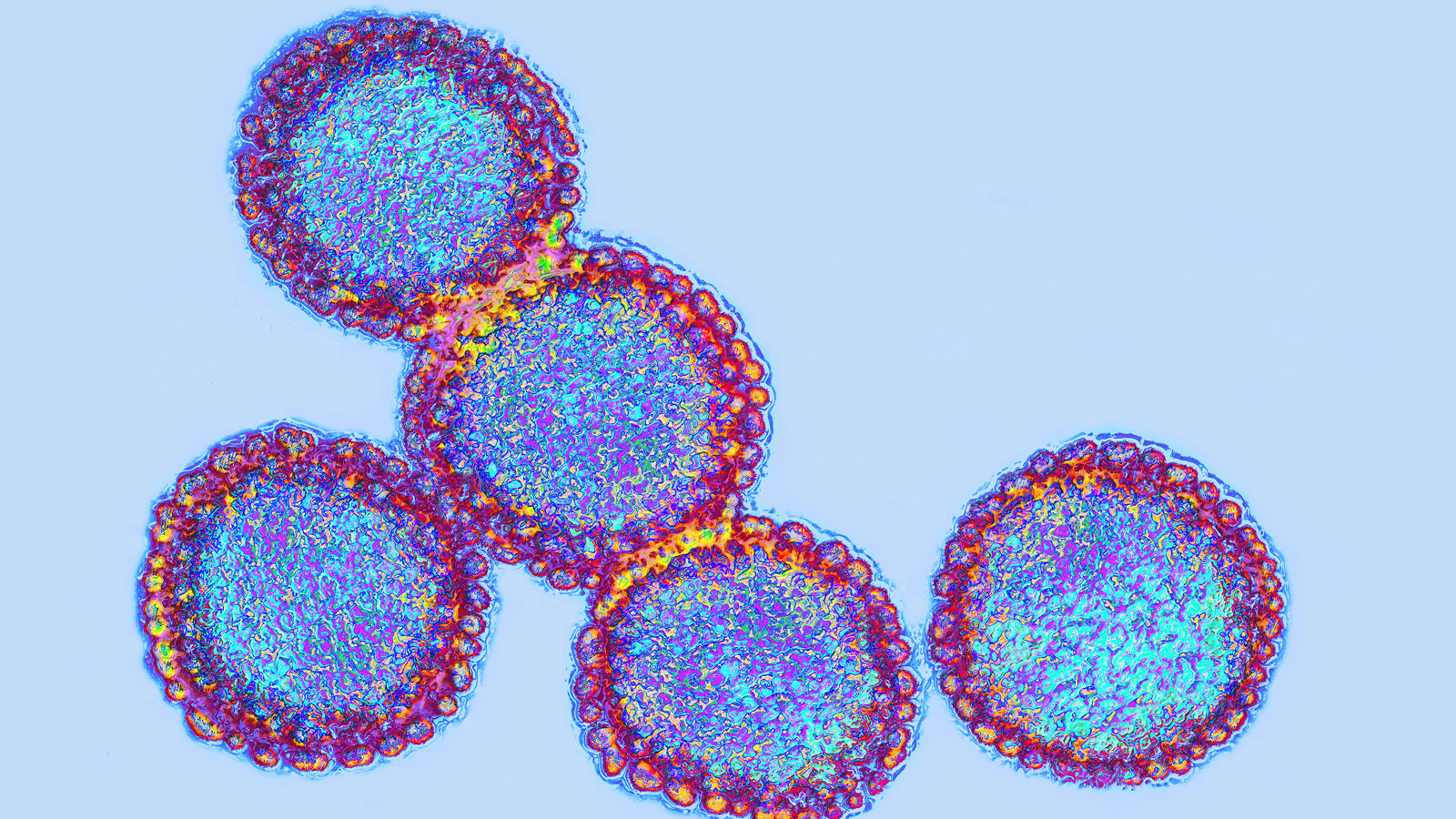
Lactose intolerance is usually the result of your body not producing enough lactase – a digestive enzyme that breaks down lactose molecules to glucose and galactose. When undigested, or partially digested, lactose passes into your colon, where it’s broken down by gut bacteria. This process increases the amount of fluid and gas in your gastrointestinal system.

There are a few reasons why people develop lactose malabsorption. According to a review published in the Nutrients journal, the most common cause is rooted in genetics. In some people, genes responsible for the production of lactase do not work properly. These faulty genes can lead to lactase non-persistence (also referred to as primary lactase deficiency), a condition where lactase levels start dropping after infancy. This is why many lactose intolerance tends to be diagnosed later in life. Whereas congenital lactase deficiency, a condition in which people start experiencing the symptoms from birth, is less common.
Lactose intolerance can also be triggered by an injury to the small intestine and this condition is often referred to as secondary lactose intolerance. Infections and certain diseases, such as Crohn’s disease and celiac disease, can affect the body’s ability to digest lactose.
Lactose intolerance: Diagnosis and testing
Diagnosing a lactose intolerance involves several steps. First, your doctor will ask you many questions to get a good understanding of your personal and medical history. They will enquire about your symptoms, family history, eating habits and the kind of medications you take regularly. They may also perform a physical examination. Afterwards, your doctor will usually conduct some tests to check for lactose malabsorption and to exclude other chronic conditions which may present similar symptoms (such irritable bowel syndrome, celiac disease, or small bowel bacterial overgrowth). They may also ask you to stop eating and drinking dairy products for a period of time to see if your symptoms go away. If they persist despite changing your diet, certain additional tests may be needed to obtain a diagnosis.
The most common test used to diagnose lactose intolerance is the hydrogen breath test. When lactose is not being absorbed, it can lead to abnormally high levels of hydrogen in your breath. A medical professional will provide you with a dose of liquid drink containing a small amount of lactose. After drinking it, you will be asked to breathe into a special container every 30 minutes over a period of a few hours. During this time, your doctor will collect your hydrogen measurements and monitor your symptoms.
Another way to diagnose lactose intolerance is the milk tolerance test. During this test you’ll be given a 500ml glass of milk and your blood sugar levels will be measured afterwards. If your blood sugar levels do not rise after drinking the milk, it means that the lactose in the milk was not digested and you may be lactose-intolerant.
Can you treat lactose intolerance?
Elimination diet
To date, there is no cure for lactose intolerance. The most effective way to avoid the symptoms of this condition is to remove all sources of lactose from your diet. However, it may not be as simple as switching to dairy-free products. Lactose is a popular additive, commonly used as a filler, stabilizer and sweetener in many different packaged foods, baked goods, and infant formulas. It can be found in many salad dressings, salad creams, biscuits, cakes, chocolate, pancake mixes, instant soups and even some processed meats. This lactose is often referred to as ‘hidden lactose’.
The labeling of ‘lactose-free’ products is another issue. There is currently no universal law regulating the production of lactose-free foods, which makes it more difficult for affected customers to identify safe products. Manufacturers are not legally obliged to list lactose separately on the food label so you need to check the ingredients list for milk, whey, curds and milk products such as cheese, butter and cream.

Lactase supplements
To a certain extent, lactose intolerance can be counteracted with dietary supplements containing synthetic lactase enzymes. They usually come in the form of tablets or drops, to be taken right before you eat or drink products that contain lactose. Drops can also be added directly to dairy milk.
However, there are controversies surrounding the efficacy of lactase supplements, as pointed out by researchers from the Nutrients journal. You should consult your doctor before using these supplements.
Probiotic supplements
Probiotics are live microorganisms that may provide health benefits when consumed, mostly through restoring the gut microbiome and improving gut health. A growing body of evidence suggests that probiotic bacteria found in fermented and unfermented milk products can help to alleviate the digestive symptoms of lactose intolerance.
This is because certain probiotic strains have shown a similar enzymatic activity to lactase. Although results from studies are not consistent, probiotic supplementation tends to have a positive impact on the symptoms of lactose intolerance. Still, more research is needed to establish which types of bacteria can be effectively used.
This article is for informational purposes only and is not meant to offer medical advice.
Additional resources
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.

Anna Gora is a health writer at Live Science, having previously worked across Coach, Fit&Well, T3, TechRadar and Tom's Guide. She is a certified personal trainer, nutritionist and health coach with nearly 10 years of professional experience. Anna holds a Bachelor's degree in Nutrition from the Warsaw University of Life Sciences, a Master’s degree in Nutrition, Physical Activity & Public Health from the University of Bristol, as well as various health coaching certificates. She is passionate about empowering people to live a healthy lifestyle and promoting the benefits of a plant-based diet.