HIV Pill Seems to Succeed as a Preventative
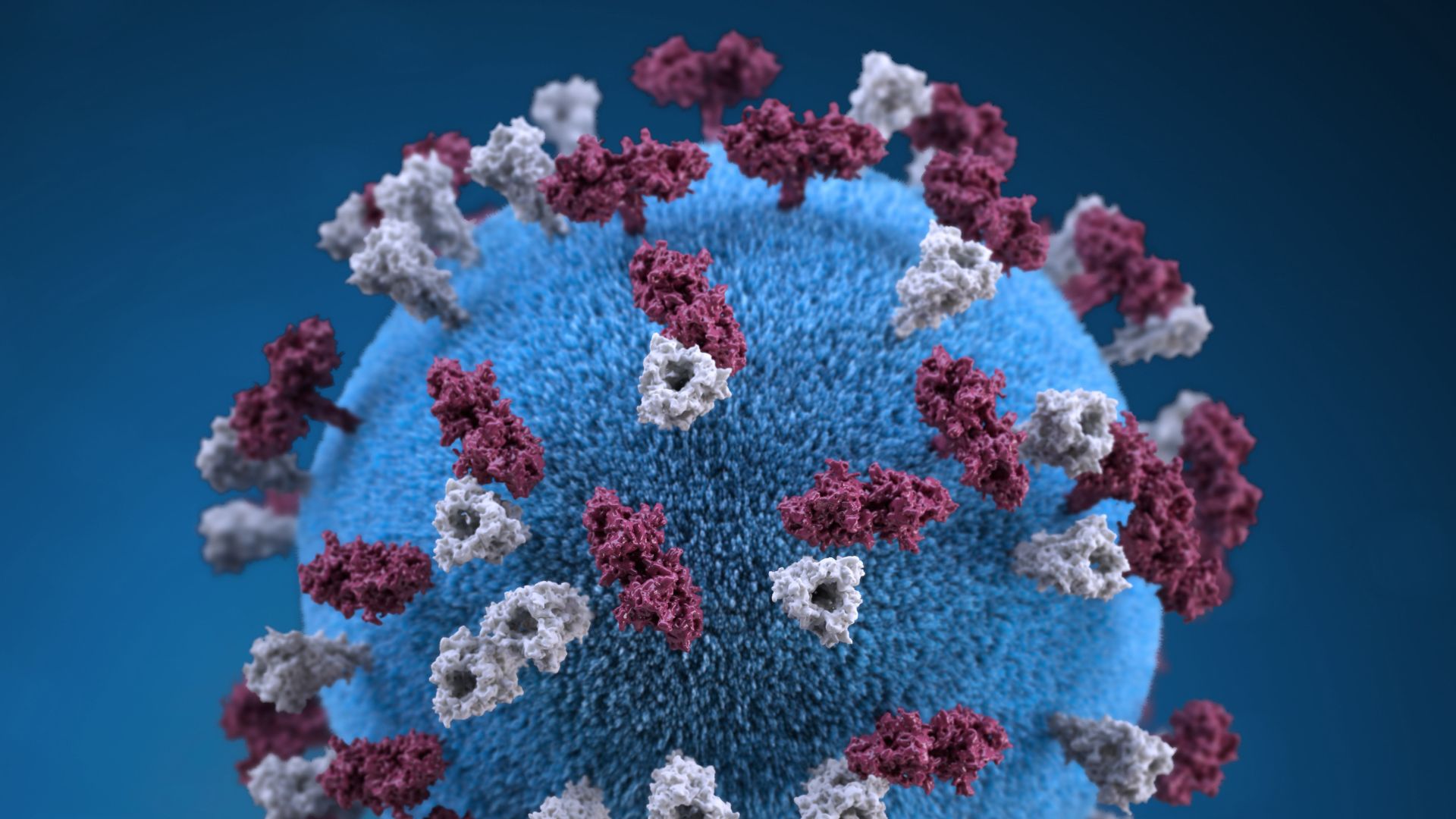
Gay men may greatly lower their chances of being infected with HIV by taking a daily dose of a drug combination commonly used as a treatment for the virus, an international study has found.
The strategy was shown to reduce the risk of acquiring HIV by 43.8 percent among men who have sex with men. And among the men in the study who adhered most closely to the regimen of taking the drug combination every day, the infection risk was reduced by even more up to 72.8 percent, according to the study.
The findings, which the National Institutes of Health called "a major advance in HIV prevention research," were the result of a large international clinical trial reported online today (Nov. 23) in the New England Journal of Medicine.
An antiretroviral tablet containing two drugs a combination of emtricitabine and tenofovir, known by the brand name Truvada was used to study the effectiveness of a preventive approach to the AIDS virus.
"We now have strong evidence that pre-exposure prophylaxis with an antiretroviral drug a strategy widely referred to as PrEP can reduce the risk of HIV acquisition among men who have sex with men, a segment of the population disproportionately affected by HIV/AIDS," said Dr. Anthony S. Fauci, director of the National Institute of Allergy and Infectious Diseases (NIAID).
More research is needed, Fauci said, to replicate the findings and to study the tablet's effectiveness in slowing HIV's spread in other groups of people, such as women and heterosexual men, Fauci said.
The study included 2,499 men and transgendered women who have sex with men. All participants were at least 18 years old and HIV-negative at the start. The study began in June 2007 and was conducted at 11 sites in Brazil, Ecuador, Peru, South Africa, Thailand and the United States.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Participants were randomly assigned either the daily antiretroviral tablet or a placebo pill. The researchers said they also counseled all participants about safe sex practices and provided condoms.
Participants were enrolled for an average of 1.2 years.
By the study's end, 100 cases of HIV infection had occurred among the participants. Of those, 36 infections occurred among the 1,251 participants who received the drug combination, compared with 64 infections among the 1,248 participants who received the placebo.
The tablet's ability to reduce the risk of HIV acquisition was greatest among those who adhered more closely to the daily regimen. Those who took the drug on at least 50 percent of the days saw 50.2 percent fewer HIV infections than those taking the placebo; those who took the drug on at least 90 percent of the days recorded 72.8 percent fewer infections.
The participants reported few side effects, and the researchers found little drug resistance had developed in those given the treatment. All participants reported a decrease in the number of their sexual partners and an increase in condom use. (Those who acquired HIV were referred for follow-up health care.)
The study "provides important evidence that PrEP works to reduce HIV infection risk among gay and bisexual men," said lead author Dr. Robert Grant of the Gladstone Institute of Virology and Immunology, in San Francisco.
Although condom use and reducing the number of partners remain the most effective ways to protect against HIV infection, pre-exposure prophylaxis could represent a major step forward for efforts to control the global epidemic , Grant said.
The researchers plan to conduct a follow-up study in 2011 in which all HIV-negative participants will be offered the drug combination for 18 months. The next study is designed to provide additional information about the drugs' long-term effectiveness and safety, as well as participants' risk behavior and pill-taking practices.
NIAID sponsored the study, which also received funding from the Bill & Melinda Gates Foundation. The study drug was donated by Gilead Sciences of Foster City, Calif.