Tests for Prostate Cancer Improving with New Technology
When 54-year-old Jeff Rolf went in for his annual physical three years ago, he did not expect to come away with news of an abnormal PSA level and, eventually, a prostate cancer diagnosis.
But the level of prostate-specific antigen (PSA) in Rolf's blood had slowly increased between 2000, the year he first took the PSA test, and 2008. Doctors became concerned not because the level was particularly high, but because it trended upward through the years.
Rolf chose to have a biopsy, which was positive for cancer. The Brecksville, Ohio, resident, a vice president of marketing at a major aerospace engineering firm, had a radical prostatectomy in 2009, and underwent radiation therapy in 2010.
"If there's a poison in your body, it's a human reaction to say, 'Get it out of me,'" Rolf told MyHealthNewsDaily.
Life-saving decisions
Rolf's life was saved because of the decisions he and his doctor made regarding the results of his PSA test. The test tells a doctor if something is abnormal with the prostate and can indicate a high cancer risk.
Doctors say the PSA test is the best thing out there for prostate cancer screening, but it's infamous for its lack of specificity. Many times, an elevated PSA level could be due to an enlarged prostate, inflammation or infection rather than cancer, said Dr. John Wei, a professor of urology at the University of Michigan Health System.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
And even if the PSA test indicates a high risk of cancer, it's unable to differentiate between a slow-growing, nonlethal cancer and that of a clinically significant cancer, Wei said.
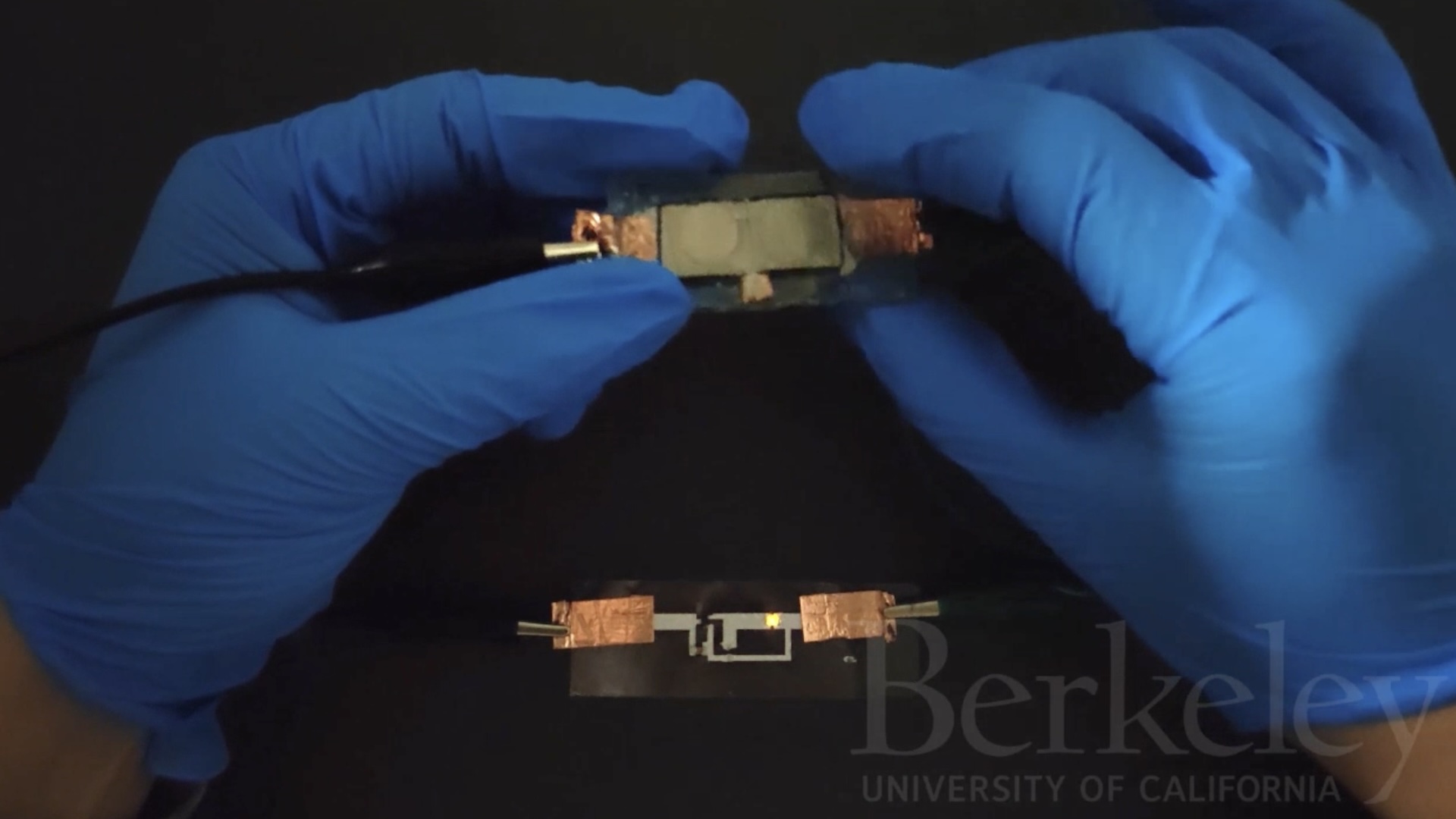
That may all change in the near future. The prostate cancer antigen-3 (PCA3) test, which is available for use but has yet to be approved by the Food and Drug Administration, measures urine levels of the genetic material mRNA. High levels of mRNA indicate an increased risk of cancer, and the results of a PCA3 test can add reliability to those of a PSA test to reduce false positives, Wei said.
And in the lab stage, a potential test measuring levels of gene fusion TMPRSS2-ERG could give doctors a better idea of whether their patient's cancer is clinically significant or not, he said.
Measuring genetic material
There were nearly 218,000 new cases and 32,050 deaths from prostate cancer in the United States last year, according to the National Cancer Institute. The cancer usually affects older men, and PSA tests are the main way of screening for the cancer.
There is no government-recommended age to start screening for prostate cancer, but doctors generally agree men should start at age 40 or 50, according to the NCI.
When Wei sees an abnormal PSA level, he doesn't tell his patient that he has cancer he simply says there's an elevated chance of cancer. The patient can then choose whether or not to undergo a biopsy of the prostate, which has its own small risks.
The chance of finding prostate cancer among men with elevated PSA levels is about one in three, but "the problem is the other two men who don't have cancer get a biopsy, perhaps unnecessarily," he said.
"When you multiply that for a million biopsies each year, that's a lot of men," Wei told MyHealthNewsDaily.
Everything on the market now for prostate cancer screening is a derivative of the PSA test, in that those tests always look for a form of PSA in the blood, said Wei, who is also the principal investigator of a National Cancer Institute-funded clinical trial testing the effectiveness of PCA3 testing.
"But PCA3 is totally outside of the PSA box," Wei said. "This is so important because it uses a different mechanism to detect cancer risk."
The PCA3 test isn't new; research on the screening test started about 10 years ago. Several versions of the PCA3 test have been made by laboratories across the United States, but the version that's been submitted for FDA approval is manufactured by Gen-Probe, a molecular diagnostics company based in San Diego, Calif., said Michael Watts, vice president of corporate communications at Gen-Probe.
Dr. Ryan Berglund, an urologist at Cleveland Clinic's Hillcrest Hospital in Ohio, administers the PCA3 test to his patients who have had negative biopsies but also have elevated PSA levels.
"That test can be a tiebreaker when a borderline decision is being made about doing a biopsy," Berglund told MyHealthNewsDaily.
Researchers are also excited about work being done by Dr. Arul Chinnaiyan, a pathology professor and investigator at the University of Michigan. Chinnaiyan is developing a test to measure urine levels of a fusion of the TMPRSS2 and ERG genes, which is found in 50 percent of prostate cancers. The gene fusion test is still being tested in the laboratory, and has not yet entered the clinical trial stage.
Testing for the TMPRSS2-ERG gene fusion could help to differentiate between slow-growing cancers that won't kill for decades and fatal cancers that require surgical intervention or radiation, Wei said.
Prostate cancer usually strikes men in old age, so it's hard to tell whether a cancer is deadly and fast-growing enough to kill a man before he dies from other age-related causes, Wei said.
Testing for TMPRSS2-ERG could help doctors decide whether it's worth it for the patient to treat the cancer or not, he added.
Looking into the future
It's impossible to predict when the FDA will approve the PCA3 screening test, according to Gen-Probe. But because screening tests are not the same as drugs, doctors are still able to use versions of the PCA3 test with the caveat for patients that even though it isn't yet FDA-approved, it has been shown to work in clinical trials.
One such trial, the results of which were published last year in the journal European Urology, followed 721 men who received biopsies for prostate cancer. Among the men with a PSA level of 3 nanograms per milliliter (what some doctors consider to be a "biopsy-able" level), 64.7 percent of prostate cancers were missed, said study researcher Monique Roobol, of the Erasmus Medical Center in the Netherlands.
But in that same group of men, the PCA3 test missed only 32 percent of prostate cancers, Roobol said.
Even though study results are promising, the "test needs to be further evaluated in an unbiased setting and it has to become clear that the test results are stable and reproducible," Roobos told MyHealthNewsDaily.
PCA3 tests may be the closest to entering regular clinical practice, but there are many other biomarkers tested in labs around the world that could also predict prostate cancer risk , said Dr. David Quinn, medical director of the Norris Cancer Hospital at the University of Southern California.
Some of these biomarkers include prostate stem cell antigens, which are proteins associated with cancer, and human kallikrein 2, which is very similar to PSA, Quinn said.
However, it's not likely that any of these tests will ever replace the PSA test they would simply increase the reliability of PSA, he said.
"There will be an improvement of the PSA assays that I don't think will be entirely good enough to knock PSA out, but we may end up with five or so related molecules in that spectrum that may tell us more than if we just did a test on the PSA levels," Quinn told MyHealthNewsDaily.
Pass it on: Tests that measure levels of prostate-specific antigen in men's blood are vital for prostate cancer screening. But there are other tests on the horizon that can reduce the number of false positives and better inform doctors on the aggressiveness of the cancer.
- 7 Diseases You Can Learn About From a Genetic Test
- The 10 Deadliest Cancers and Why Thereâ??s No Cure
- Top 10 Leading Causes of Death
Follow MyHealthNewsDaily staff writer Amanda Chan on Twitter @AmandaLChan.