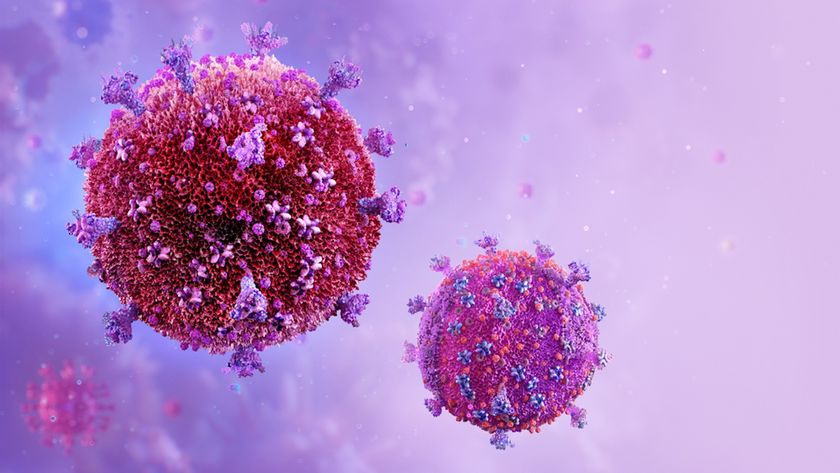
Proposed HIV Treatment Could Hitchhike with Virus
A major obstacle in attempting to suppress the HIV epidemic has been getting treatments to high-risk groups, such as intravenous drug users, who account for most of the disease spread. A newly proposed, although theoretical, therapy for HIV would get around this problem with a unique strategy the use of HIV itself as a way to transmit the treatment.
The therapy uses synthetic, virus-like particles that both reduce the amount of HIV in the body, and tag along with HIV to spread between individuals. In other words, individuals acquire both the disease and the remedy at the same time.
Using a model to simulate the outcomes of such a therapy, the researchers found these particles, known as therapeutic interfering particles (TIPs), could lower infection rates better than current drugs or proposed vaccine treatments alone.
TIPs would not replace current treatments, but rather work with them to reduce the disease prevalence, the researchers say.
However, the technique is still hypothetical at this point, and much more research needs to be done to determine the true efficacy of TIPs, said study researcher Leor Weinberger, a biochemist at the University of California, San Diego. For instance, researchers need to determine whether TIPs do in fact transmit reliably. While TIP prototypes have been created, the researchers have yet to test them in animal models.
There are also ethical concerns regarding a therapy that can transmit disease between individuals. "I am not sure that our society and our medical community is ready to accept a [therapy] that is transmissible that is based on HIV," said Vicente Planelles, a microbiology and immunology researcher at the University of Utah, who was not involved in the study.
A transmissible therapy
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
TIPs are basically minimal versions of the HIV virus itself. In order to replicate inside cells, infect new cells and transmit between individuals, TIPs rely on components provided by HIV. In essence, TIPs are parasites of HIV, Weinberger said. "It's basically a virus of the virus," he said.
By using up HIV's resources, TIPs could theoretically reduce a person's "viral load," or amount of virus in the body, to a point where the virus is far less of a threat to health.
A model developed by the researchers showed TIPs could lower the prevalence of HIV in sub-Saharan Africa by 30-fold in 50 years. For comparison, antiviral drugs or vaccines alone could only lower the prevalence less than twofold in 50 years, the researchers say.
TIPs are so effective because they can penetrate high-risk populations, including intravenous drug users and commercial sex workers, who are responsible for a disproportionate amount of disease transmission, the researchers say.
"I think that the conclusions that they reach are reasonable, although, of course, theoretical," Planelles said.
Some argue that the model is based on many assumptions that researchers still do not have data to back up, said Sally Blower, biomathematician and evolutionary biologist at the University of California, Los Angeles, who was not involved in this study.
Weinberger said the main point of the study is not to prove efficacy, but rather show such a therapy might be worthwhile to research.
"We're not saying 'Deploy this,'" Weinberger said. "We were asking, is this worth pursuing? And we think the answer is yes."
Ethical concerns
An advantage of TIPs compared with current drugs is that TIPs evolve along with HIV, which means HIV is less likely to develop resistance to them.
But evolution can also be dangerous. There's a chance TIPs could change in a way that would be harmful.
"We need to be very cautious about what can happen because there's always unpredictables," Planelles said.
There is some precedent for having a transmissible therapy, Weinberger said. People who receive the live polio vaccine can shed the virus and transmit immunity to others.
Some point out that this therapy can also integrate into a person's DNA.
"[It's] unclear if any regulatory agency would allow one to produce a transmissible therapy that will be transferred to another individual and then integrate into the genomes of cells in the recipient," said Jerome Zack, a researcher at the UCLA, who studies HIV infection but was not involved in the current study.
Weinberger is collaborating with bioethicists to explore these ethical issues.
The study was published online March 17 in the journal PLoS Computational Biology.
Pass it on: A theoretical way to fight HIV would be to use a therapy that would transmit along with the virus in order to reach high-risk groups.
- 5 Dangerous Vaccination Myths
- Cure for HIV Claimed But Not Proven
- AIDS: A 'Winnable' Public Health Battle?
Follow MyHealthNewsDaily staff writer Rachael Rettner on Twitter @RachaelRettner.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.