Male Infertility Could Be Cured in Future, But Hurdles Remain

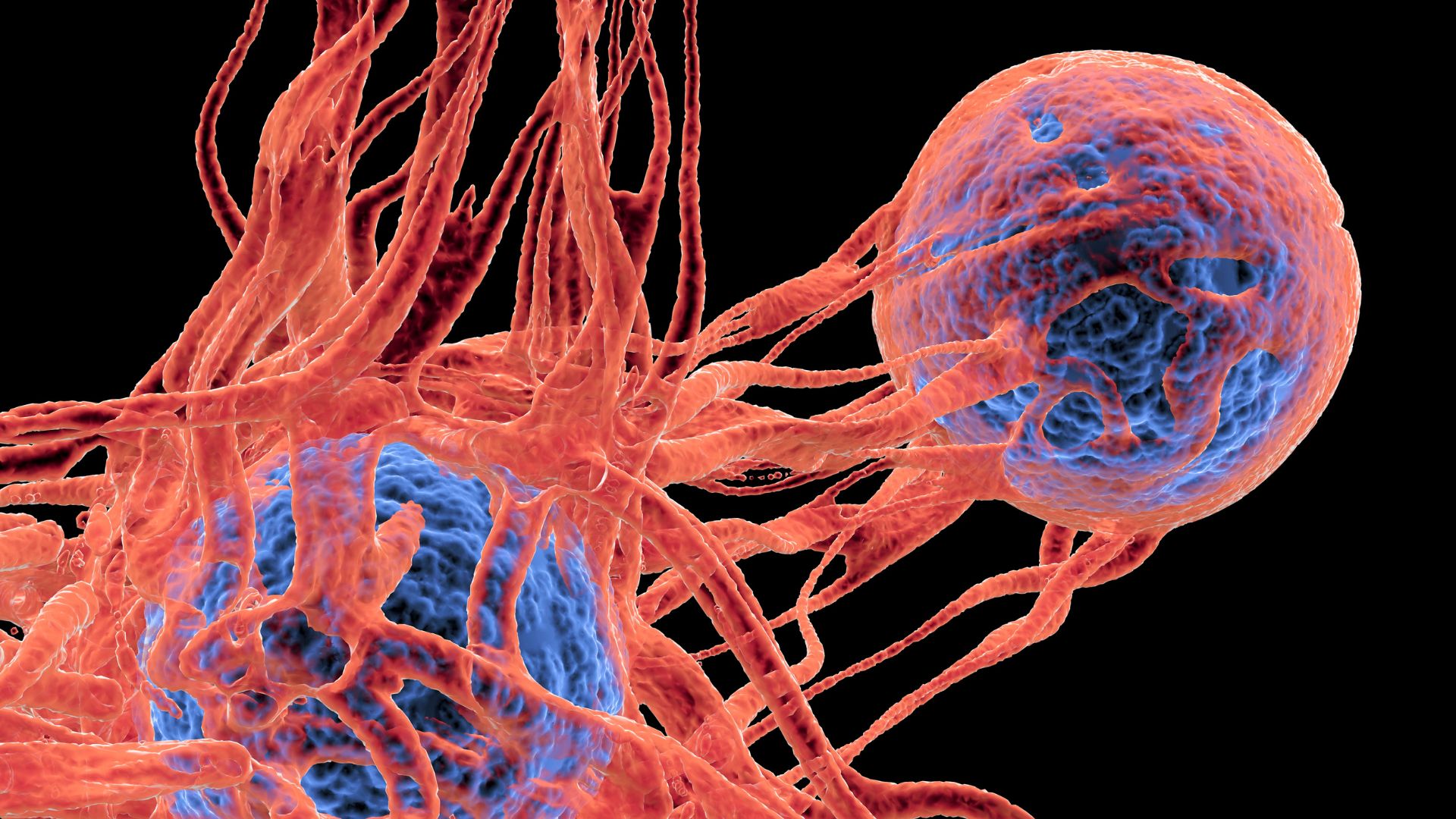
A number of recent studies have suggested that some types of male infertility will soon become a thing of the past —researchers in Israel grew mouse sperm from testicular cells in a lab, and researchers in Japan created living mice offspring from stem cells that were grown into sperm in the testicles of previously infertile mice.
The research has been a source of optimism, spurring hopes that men whose infertility stems from an inability to produce healthy sperm — which is about 1 percent of all men trying to have children— will be able to have children.
However, a number of hurdles remain to bringing the possibility of treatment for infertility in men, and researchers were reluctant to give a timeline for when infertile men might expect a treatment.
"I can't estimate the period," said Mahmoud Huleihel, a professor of immunology and microbiology at Ben Gurion University of the Negev in Israel, and senior author on that study. "It depends how the research develops, since there are a lot of limitations."
Similarly, Dr. Mitinori Saitou, a professor of anatomy and cell biology at Kyoto University in Japan and senior author on that paper, told MyHealthNewsDaily, "Our research is still at a purely basic level, using the mouse as a model," and it would take many more years to use human stem cells to make human sperm.
Making sperm in a lab
Saitou's research generated live mouse offspring from sperm made from both embryonic stem cells, and from adult stem cells that had been modified to a state where they resemble embryonic stem cells.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Such modified adult stem cells would be necessary for an infertile adult male to have a biological child. However, the researchers were successful in fewer than 20 percent of their attempts to produce offspring from those cells, and some offspring developed complications such as neck tumors.
Given the state of that research, it's "still a long ways off" before infertile men might be able to have a biological child using that method, said Dolores Lamb, president of the American Society for Reproductive Medicine and a professor of urology and molecular and cellular biology at the Baylor College of Medicine.
Instead, the method of the Israeli researchers — growing sperm from testicle cells — may hold more promise for men who are infertile, Lamb said.
"It certainly is an interesting paper, it's a well-done paper, and it's an encouraging paper," Lamb said.
Still, the researchers were not able use the sperm they grew in a lab dish to fertilize an egg.
"They don't have a live mouse to show from it," Lamb said.
Lamb said that while this research is certainly not at a point where infertile men could expect any sort of treatment. It may be relevant for boys with cancer who are not yet producing sperm that could be frozen. Tissue from their testes could be frozen now and used later, in the event they become infertile from treatments.
"Today, it's reasonable to take a testis biopsy from these patients and freeze them, because I believe the technology should be available within ten years," to produce sperm cells from testis tissue, she said.
But, she cautioned, "there's no guarantees."
In such a case, she said, it would have to be done as part of a study, because of the experimental nature and the ethical issues that might arise.
If the young patient dies, Lamb said."The parents may want to use their dead child's sperm with a surrogate, which raises huge ethical issues. A patient may not have expressed his desire to father a child posthumously, yet a spouse or partner or surrogate may want to use the sperm."
Are men necessary?
The research has led some to speculate that the production of sperm from stem cells could eliminate the need for a male partner in reproduction — theoretically, female stem cells could be used to generate sperm.
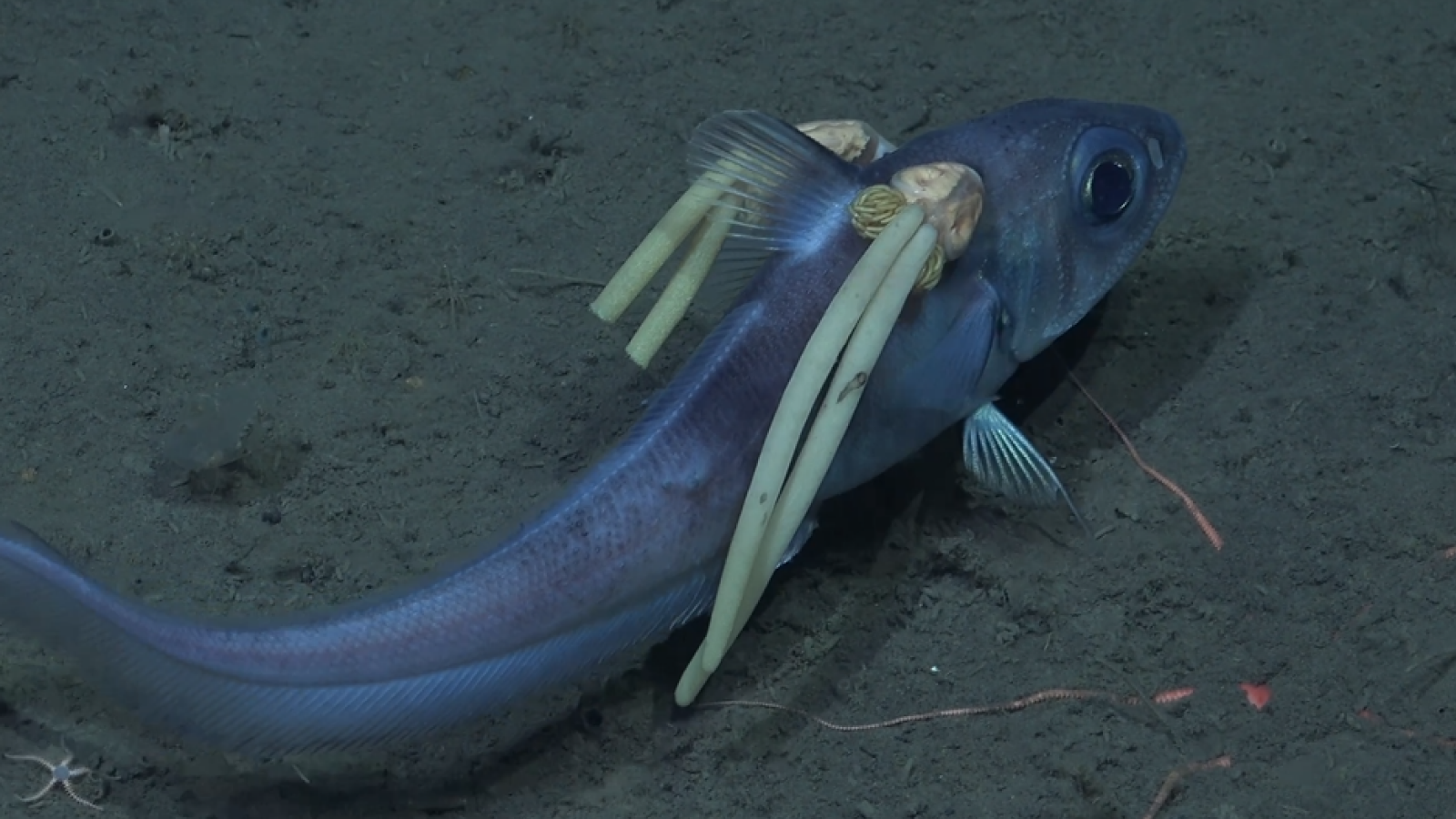
However, that speculation ignores three steps that are essential to the process, and require a male. First, while the precursors of sperm have been grown in lab dishes, testicles have been needed to grow them fully. The researchers at Kyoto University, in the only lab thus far that has produced healthy offspring from lab-grown sperm, found they needed to grow those sperm in functioning testes.
A second issue has been that cells from women have not been able to mature into functioning sperm."The presence of two X chromosomes is problematic," in the formation of sperm cells, Lamb said.
Finally, because of the way DNA naturally combines in reproduction, a male and female are necessary. After fertilization, in a process known as imprinting, the DNA is marked for functioning in the offspring.
Imprinting occurs differently depending on whether a DNA strand has come from a woman or a man. DNA combined from two women (or two men) would not be imprinted properly, and the resulting embryo would not survive.
"Any time you do something 'unnatural,' it's hard to get it to work, it's a complicated, complex process," Lamb said.
The paper from Kyoto University was published on Aug. 19 in the journal Cell. The paper from Ben Gurion University of the Negev was published in the November issue of the Asian Journal of Andrology.
Pass it on: Scientists are getting closer to finding a way to help infertile men have children, but a solution is still a long way off.
Follow MyHealthNewsDaily on Twitter @MyHealth_MHND. Find us on Facebook.
Is getting an IUD painful?
'Useless' female organ discovered over a century ago may actually support ovaries, study finds