5 Ways Gut Bacteria Affect Your Health
Introduction
Although you might like to think of yourself as your own person, you actually share your body with many millions of bacteria.
In fact, it's estimated that the human gut contains 100 trillion bacteria, or 10 times as many bacteria as cells in the human body.
These bacteria, or gut flora, influence health in many ways, from helping to extract energy from food to building the body's immune system, to protecting against infection with harmful, disease-causing bacteria.
Researchers are only just beginning to understand how differences in the composition of gut bacteria may influence human health. From what we know so far, here are five ways gut flora affect wellness:
Obesity

A growing body of research suggests that gut bacteria influence weight. One recent study found that obese people have a less diversity in their gut flora than lean people. Other studies have suggested that an increase in a group of gut bacteria called Firmicutes, and a decrease in a group of gut bacteria called Bacteroidetes, are linked with obesity.
Research done on animals may provide clues about how gut bacteria affect weight gain. One recent study found that mice that received a "gut bacteria transplant" from an obese person gained more weight and fat mass than those who received bacteria from a lean person.
What's more, the transplant altered the metabolism of the mice: animals that received gut bacteria from an obese person had metabolic changes linked with obesity in humans (such as increased production of compounds called branched-chain amino acids); while those that received gut bacteria from a lean person had metabolic changes linked with reduced body weight (such as increased breakdown of carbohydrates).
Heart disease

When gut bacteria feed on certain foods — including eggs and beef — they produce a compound that could boost the risk of heart disease, according to a recent study.
Participants in the study with high levels of the compound, called trimethylamine-N-oxide (TMAO), in their blood were 2.5 times more likely to have a heart attack, stroke or to die over a three-year period compared with people with low levels of the compound.
Although the findings are preliminary, the results reinforce existing dietary recommendations for lowering heart disease risk, which advise people to reduce consumption of foods high in fat and cholesterol (such as beef and eggs), the researchers said.
Immune system
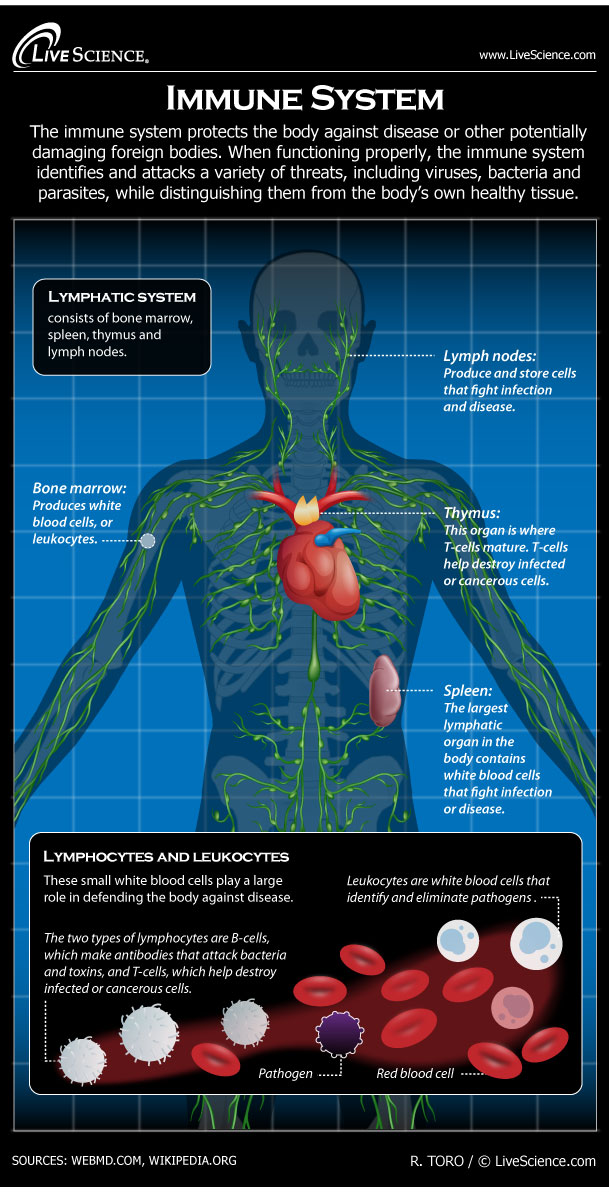
Your gut is the main area in the body where the immune system interacts with what's brought in from the outside world. Thus, the interaction between gut bacteria and your own cells appear to play an important role in the development of a fully-functioning immune system. According to a 2003 review paper in the Lancet, lymphatic tissue in the intestine contains the largest pool of cells capable of producing an immune response.
A 2012 study found that whether babies are fed breast milk or formula influences the composition of their gut bacteria, and in turn, the development of their immune system. Babies fed only breast milk had more diversity in their gut bacteria than babies who were fed only formula. There was also a link between the genes that were "turned on" in the babies' gut bacteria, and the genes that were "turned on" in their immune system.
Brain

Disrupting gut bacteria may have an effect on the brain, and in turn, behavior, studies in animal suggest.
A 2011 study in mice found that animals given antibiotics (which kill gut bacteria) became less anxious, and when their gut bacteria was restored, so was their anxiety.
Mice given antibiotics also showed changes in their brain chemistry that have been linked to depression.
The researchers said they suspect the bacteria are producing chemicals that can access and influence the brain.
If gut bacteria play a role in human behavior, its possible that therapies that aim to restore normal gut flora, such as probiotics, may be helpful in correcting behavior and mood changes in people with gastrointestinal diseases, according to the researchers. However, it's not clear if the results apply to people.
Infant colic

Abnormal gut bacteria in infants may be one cause of colic, or excessive crying, recent research suggests.
In the study, colicky babies (who cry for more than three hours a day without a medical reason) had a distinct bacterial "signature": They had higher numbers of bacteria from a group called Proteobacteria in their guts compared to babies without colic.
Proteobacteria include bacteria known to produce gas, which may cause pain in infants and lead to crying, the researchers said.
These abnormities disappeared after the first few months of life, which suggests they are temporary. However, this study was small and conducted for just a few months, so additional, longer studies are needed to confirm the results.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.