Dr. DNA: Using Genes to Guide Prescriptions

Your genes determine the color of your eyes and whether you have dimples or can roll up your tongue. They control plenty of features inside your body, too, including how you respond to certain medicines.
In general, each gene is the body’s instructions for building a specific protein. These instructions are in a code made up of biochemical units abbreviated A, T, G and C.
Different people might have slightly different versions — or spellings — of genes. Most of these variations have no effect on health. But if a gene codes for a protein that plays a role in how the body responds to medications, people with an unusual spelling might find that medications work differently or cause side effects not experienced by people with a more common spelling.
Scientists in a research field called pharmacogenomics aim to understand how genes influence individual drug responses. Many of these researchers are supported by grants from the National Institutes of Health. The scientists’ goal is to provide information that helps doctors prescribe the drug and dosage that would work best for each person.
Here are examples of NIH-funded pharmacogenomics research findings related to different medical conditions. Not all have made it to routine use in doctors’ offices, but the use of genetic information to guide treatments is growing.

Heart Attacks and Strokes
For people who have had a heart attack or stroke, doctors often recommend daily doses of aspirinto lower the risk of recurrence. Aspirin works by reducing the activity of blood-clotting particles called platelets. Excess platelet activity can cause blood clots that lead to heart attacks and strokes.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
About 60 million Americans take aspirin each day to prevent such problems. But in 10 to 30 percent of these people, it doesn’t work. A team of researchers discovered a set of 60 genes whose activity can predict whether a person will benefit from aspirin therapy or not.
A different group of researchers focused on a gene called PEAR1, which codes for a protein on the surface of platelets. One spelling of the gene, with an A instead of a G at a particular spot, makes people more likely to have a heart attack, even while taking aspirin. For these people, doctors can prescribe other methods to prevent heart attacks and strokes.
Lung Cancer
Lung cancer is the number-one cause of cancer deaths in both men and women in the United States, and smoking leads to 80 to 90 percent of these cases. Smokers who can’t quit might benefit from research on a gene called CYP2A13. This gene codes for a lung enzyme that converts a substance in tobacco into two cancer-causing molecules.
Scientists plan to explore whether blocking the activity of CYP2A13 could prevent the formation of these dangerous molecules and reduce the incidence of lung cancer among smokers.
Breast Cancer
For some women at high risk for breast cancer based on their age, family medical history or other factors, a long-term treatment with a class of drugs called selective estrogen receptor modulators (SERMs) can cut the disease risk in half. Researchers recently discovered that women have the greatest chance of benefitting from the strategy if they have certain spellings in two locations—the ZNF423 gene and near the CTSO gene.
In the largest-scale analysis of its kind, such women were almost six times less likely to develop breast cancer during the 5-year course of treatment than were women with neither advantageous spelling. With this information, women and their doctors will be better able to balance the potential benefits and risks of the long-term preventive strategy.
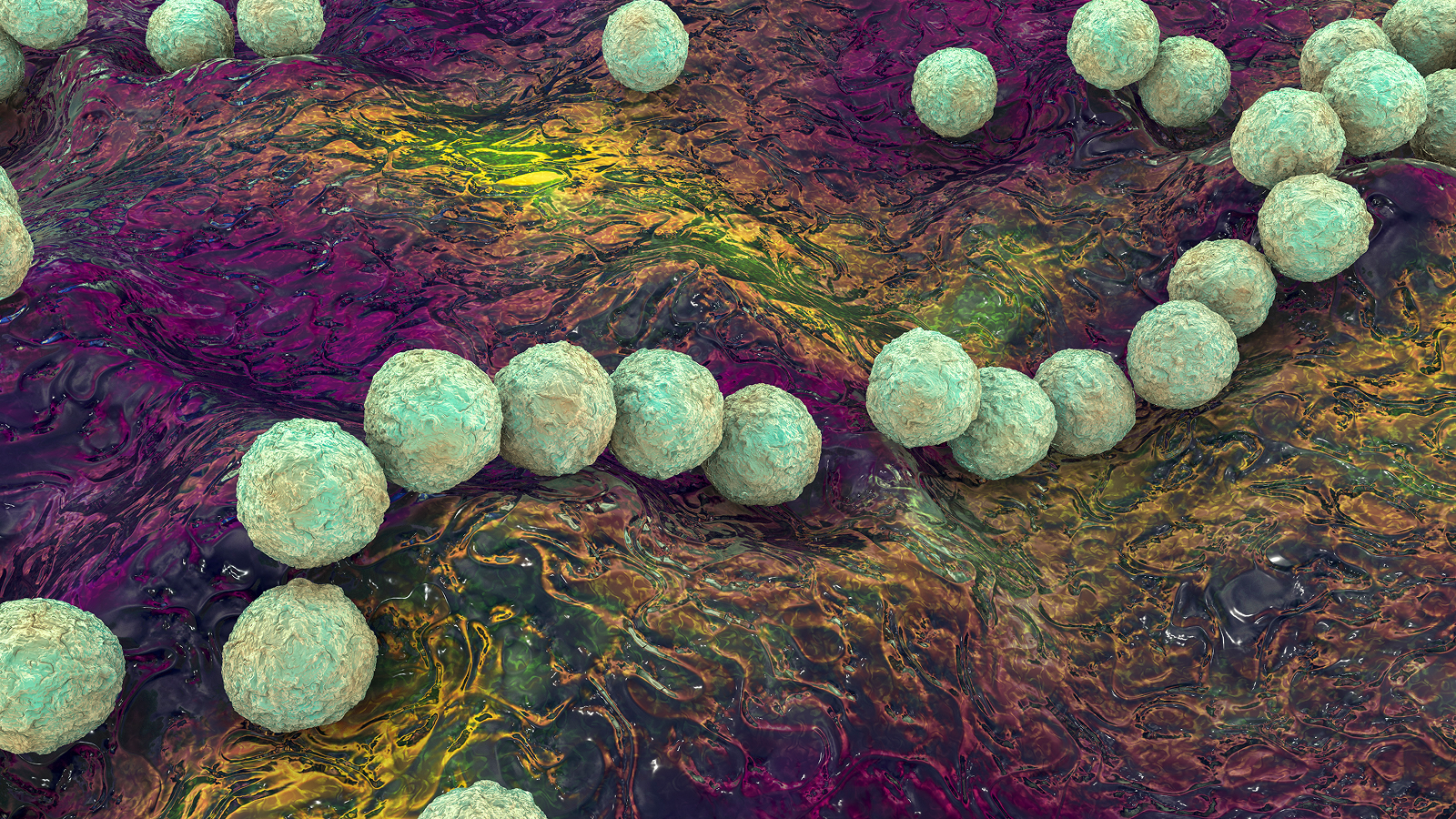
Childhood Leukemia
Drugs known as thiopurines are prescribed for a childhood cancer called acute lymphoblastic leukemia (ALL), but getting the dose right is critical. To help them do so, doctors can examine the genetic spelling of a protein called TPMT in each patient. TPMT processes and inactivates thiopurines.
The most common genetic spelling of TPMT makes a protein that acts on thiopurines quickly. But about 10 percent of people have a variant spelling that produces a slower-acting protein. For these people, doctors can prescribe lower thiopurine doses—or different medications—to prevent the drug from building up to toxic levels before it’s processed by the body.
Rheumatoid Arthritis

Rheumatoid arthritis causes swelling and pain in a person’s joints, usually in the hands and feet. It happens when the body’s immune system mistakenly attacks the joints using an arsenal of inflammation-producing molecules. Decades ago, researchers discovered that blocking a single molecule, TNF-alpha, could turn down this inflammatory response. Now, medicines that turn off TNF-alpha are used to treat rheumatoid arthritis and a number of related disorders.
Scientists found that the effectiveness of a TNF-alpha blocker called etanercept depends on the spelling of a gene called CD84. For two other TNF-alpha blockers, the spelling of CD84 doesn’t matter. This discovery will help researchers understand differences in how the three drugs work in the body, possibly paving the way for personalized prescriptions based on an individual’s version of CD84 or other genetic factors.
These and other studies will continue to yield insight into the complicated process of how our bodies respond to medicines and point to new ways to tailor therapies for each person.
This Inside Life Science article was provided to LiveScience in cooperation with the National Institute of General Medical Sciences, part of the National Institutes of Health.
Learn more:
Frequently Asked Questions About Pharmacogenomics
Medicines by Designbooklet
Also in this series: