
Why is a Common Hip Problem So Frequently Misdiagnosed? (Op-Ed)

Dr. Thomas Ellis is an orthopedic surgeon at The Ohio State University Wexner Medical Center. Ellis contributed this article to LiveScience's Expert Voices: Op-Ed & Insights.
Femoral acetabular impingement. You may not have heard of it, but it's a hip problem many people across the United States are dealing with.
Hip pain is traditionally associated with older adults, but everyone from young athletes to "weekend warriors" and even non-athletes can be at risk for developing this hip problem. Last month, Oakland University announced basketball senior forward Raphael Carter will undergo surgery for hip impingement and will miss the season. University officials reported that he had been waiting over the summer to finally get the correct diagnosis. Many people suffering with hip pain may have femoral acetabular impingement and not realize it.
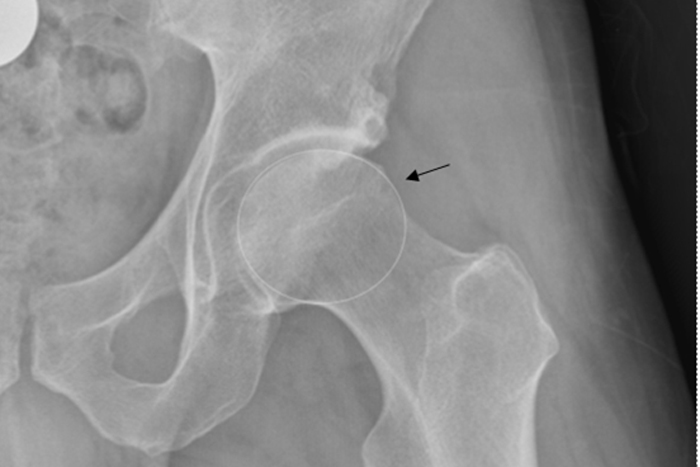
Femoral acetabular impingement (FAI) is a condition where the bony parts of the hip joint are misshapen. As a result, the ball of the femur (the top part of the thigh bone) does not fit perfectly in the acetabulum (hip socket). This causes friction in the joint and often results in tearing of the hip labrum (the cartilage that seals the socket). As the hip flexes and rotates, the front of the ball hits the front of the socket causing a collision known as an "impingement." Over time, repeated collisions of the ball with the front of the socket can tear the labrum and damage the adjacent cartilage, resulting in pain and loss of function.

Symptoms may include pain in the hip (often felt in the groin), clicking within the joint, giving way (the leg just 'gives out'), discomfort when moving the hip into certain positions (especially lifting the knee up and rotating the leg inwards), stiffness of the joint, and difficulty walking, turning, climbing steps or running.
I treat many patients with these symptoms who have an incorrect diagnosis. FAI is commonly misdiagnosed because it affects many different ages and types of people. I've treated patients with FAI as young as twelve up to those in their fifties and even sixty years old. The condition can develop gradually, starting as a little twinge with specific movements, then progress to daily pain over a long period of time, or it can start after a traumatic injury like a fall or a car accident.
Identification of FAI is challenging and symptoms are commonly confused with other hip problems. Often people with FAI will be diagnosed with another condition such as a groin pull, arthritis, bursitis, dysplasia, low back pain, a pinched nerve or tendinitis, among others. Recreational and competitive athletes involved in sports like football, soccer, hockey, basketball and dance are at risk of developing this condition due to repetitive, high-demand hip movements, but non-athletes can feel hip pain from FAI too.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
For many patients, even routine daily activities — like a long car ride or bending and lifting an object — can be painful. I often see patients who say they've been searching for their symptoms online because they don't feel they've been diagnosed correctly. Eventually, they find a hip specialist who can look at patient symptoms, physical examination and specialized imaging of the hip — to make the correct diagnosis.
Once FAI has been diagnosed, patients need to understand various treatment options. I always start with non-operative options first. It's important to understand that FAI is not a condition which always requires surgery. A good first step is to start with a course of physical therapy. The physical therapist shows the patient what movements to avoid, how to sit correctly to alleviate hip pain, and how to vary exercise routines to reduce symptoms. This might be as simple as doing a different cardio exercise or modifying a weight-training routine. The therapist will assess — usually within three to four visits — whether continued therapy is likely to improve symptoms. People whose muscles are weaker often benefit from physical therapy, even if they end up having surgery later. Therapy strengthens the muscles around the hip and abdomen, which aids recovery after surgery.
If a patient does not respond well to therapy and activity modifications, we consider further treatment options, including surgery. The goal of surgery is to reshape the bones of the hip joint to prevent the impingement of the ball on the socket. In the past, labral tears were treated with removal of the torn part of the labrum, but my approach is to to repair the labrum whenever possible. The goal of the reshaping and repair work is to restore and preserve the hip anatomy, giving the patient the best chance of avoiding early arthritis and hip replacement, or other future hip problems.
Until recently, these procedures were performed through large incisions and required cutting the hip bone and dislocating the hip. However, we now complete these procedures arthroscopically using small incisions to place a camera inside the hip joint to guide the repair work.
Hip arthroscopy is similar in many ways to surgeries for knee and shoulder injuries. Since the surgery is minimally invasive, recovery time is reduced and patients go home within a day of the surgery. Rehabilitation time is also shorter and patients avoid some complications associated with the larger incision approach.
After the procedure, patients are instructed to use crutches for the first couple of weeks. Patients also begin physical therapy to improve strength and flexibility. Many people can go back to lighter work or school activities after one to three weeks, however, it typically takes as many as sixteen weeks to return to a full level of activity. By three to six months most patients have minimal soreness or pain with physical activity, but every patient recovers at a different rate, so it's important to follow up regularly with your physical therapist and surgeon so they can carefully monitor your recovery.
If you have hip symptoms that match FAI symptoms, or have received other diagnoses in the past but aren't getting better, its a good idea to consult a specialist who treats FAI. This will allow you to be thoroughly evaluated and treated with an individualized plan. Treatments are now available which can greatly improve quality of life and restore function.
The views expressed are those of the author and do not necessarily reflect the views of the publisher. This version of the article was originally published on LiveScience.









