Brain-Machine Interface Puts Anesthesia on Autopilot

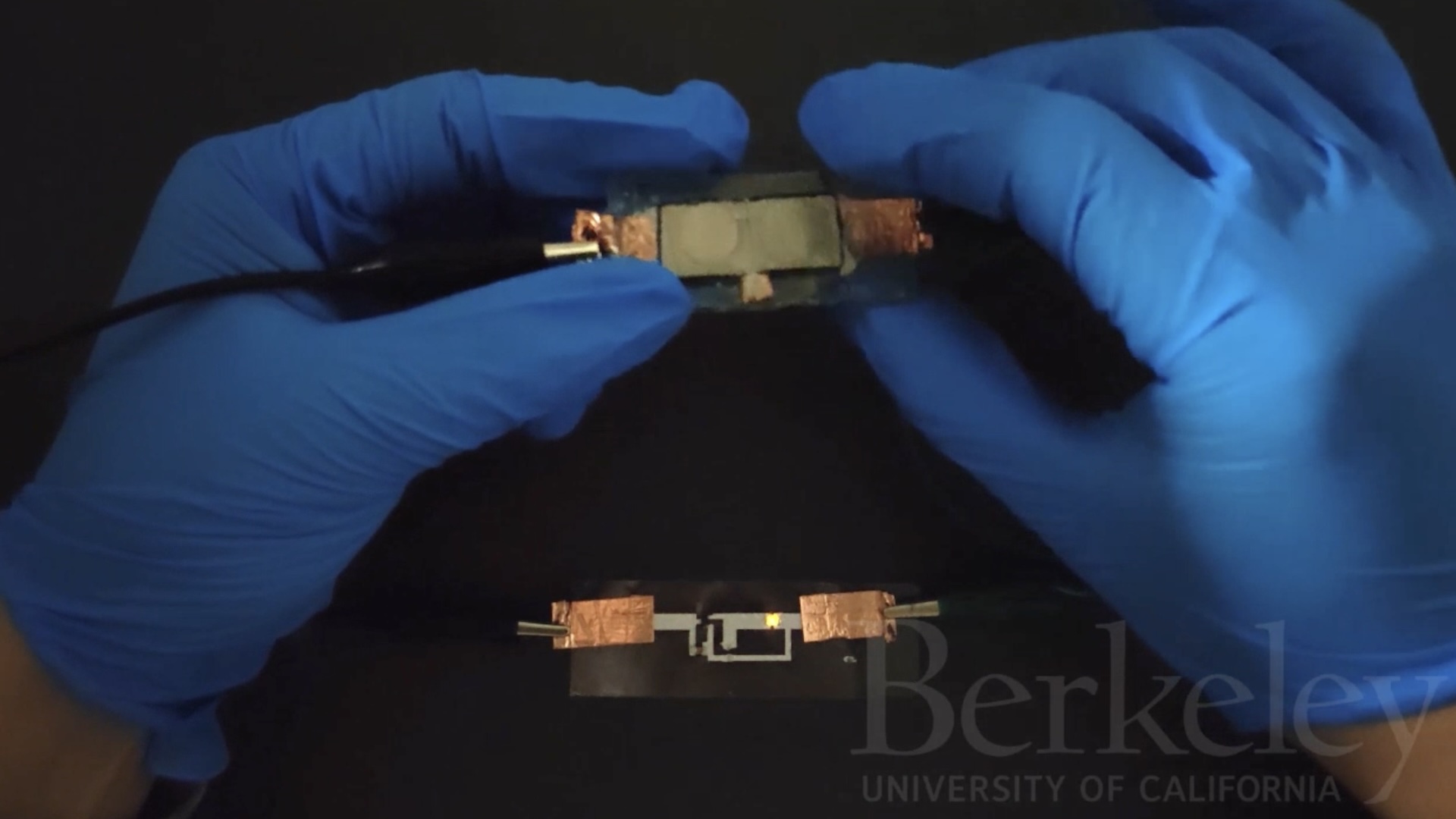
A new brain-machine interface could replace human administration of anesthetics to patients in a medically induced coma.
The machine monitors a patient's brain activity and automatically delivers just the right amount of anesthetic to keep the patient in a coma — thus reducing the amount of anesthetic needed and preventing an overdose, researchers say. Doctors could also use the system to awaken patients periodically from a coma to do neurological assessments.
In a medically induced coma, physicians administer drugs to inactivate a patient's brain, usually to treat high pressure in the skull or uncontrollable epilepsy. Doctors maintain these comas, which often last for several days, by monitoring a patient's electroencephalogram (EEG) brain activity and delivering a precise dose of anesthetic.
Controlling the delivery of the anesthesia by hand is a bit like flying a plane manually for several days, the researchers say. In contrast, the brain-machine interface puts the process on autopilot.
Doctors need to deliver enough anesthetic to maintain a level of burst suppression, a pattern of brain activity involving bursts of electrical signals followed by quietness, in order to achieve a coma state.
A team of researchers from Cornell University, Massachusetts General Hospital and MIT developed the brain-machine interface that controlled burst suppression in rodents. The system, detailed Oct. 31 in the journal PLOS Computational Biology, uses sophisticated algorithms that measure the EEG brain activity, estimate the burst-suppression level and use that information to control the release of anesthetic, in real time.
The machine's developers say it could be adapted for other kinds of anesthesia, too. The system could replace the manual administration of anesthetic in long surgeries and intensive-care units, where patients often must be under anesthesia for days at a time.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
However, future studies will have to test the therapeutic benefits of this technology.
Follow Tanya Lewis on Twitter and Google+. Follow us @livescience, Facebook & Google+. Original article on LiveScience.