Natural Disasters Bring Risk of Fungal Infections
Natural disasters can create conditions that put survivors at risk for fungal infections, which are often overlooked, according to a new report from the Centers for Disease Control and Prevention.
Earthquakes, hurricanes, tornadoes and other natural disasters can displace harmful fungi from their natural habitat, potentially bringing them into contact with injured and vulnerable people, the report said. Individuals may inhale fungal spores, or the spores can find their way into wounds, resulting in infections.
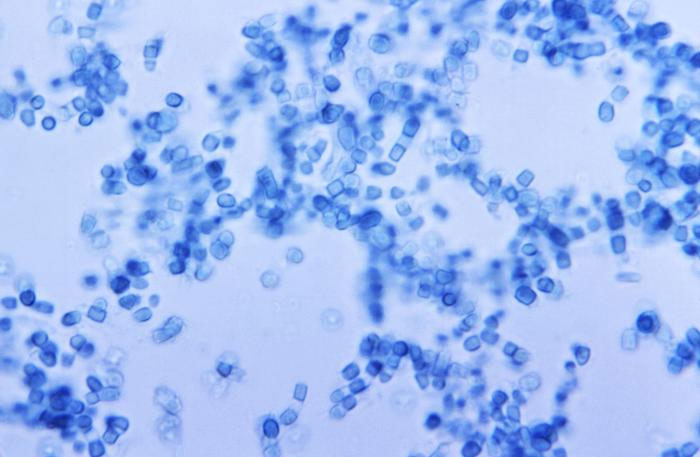
For example, after the devastating 2011 tornado in Joplin, Mo., 13 severely injured people developed a rare fungal infection called mucormycosis. The type of fungus that causes this infection is found in the soil and decaying organic matter that victims were exposed to as a result of the disaster. [Top 10 Deadliest Natural Disasters in History]
Following a 1994 earthquake near Los Angeles, more than 200 people developed a fungal infection called coccidioidomycosis, also known as Valley Fever. Landslides and aftershocks caused by the earthquake generated dust clouds, which dispersed soil fungus that people inhaled, the report said.
Although not a very frequent occurrence, fungal infections following disasters may become more common with climate change, the report said. Warmer temperatures may allow harmful fungi to expand into new areas. Coupled with the predicted increase in extreme weather, "a larger or more geographically widespread ecologic burden of pathogenic fungi could lead to greater numbers of disaster-associated fungal infections," the report said.
Health care providers should be aware of the potential for people to develop fungal infections after natural disasters, so that treatment can be started early, the report said. Fungal infections are sometimes mistaken for other illnesses, such as bacterial infections, which can delay appropriate treatment. After the Los Angeles earthquake, for example, 93 percent of Valley Fever sufferers received one or more antibiotics before their fungal infection was diagnosed, the report said.
Typically, these fungal infections are uncommon in people with healthy immune systems, so doctors may not think to look for them. So when patients have infections that are not responding to antibacterial treatments, doctors should consider fungal infections, the report said.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
The delay in getting medical treatments that often happens after natural disasters can also contribute to these infections taking hold, the report said.
"Strategies to reduce disaster-associated fungal infections should be considered within the broader context of comprehensive and sustainable risk-reduction methods to prevent disaster-related injury and illness," the researchers wrote in their report, published in the March issue of the CDC journal Emerging Infectious Diseases.
Follow Rachael Rettner @RachaelRettner. Follow Live Science @livescience, Facebook & Google+. Original article on Live Science.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.