Infection Control: Why Doctors Over-Prescribe Antibiotics (Op-Ed)

This article was originally published at The Conversation. The publication contributed the article to Live Science's Expert Voices: Op-Ed & Insights.
Health authorities have long warned that antibiotics should only be used when they’re genuinely needed, to restrain antibiotic-resistant superbugs and avoid potentially serious side-effects. But many doctors aren’t complying, with between 20% to 50% of antibiotic prescriptions deemed inappropriate, depending on the individual hospital.
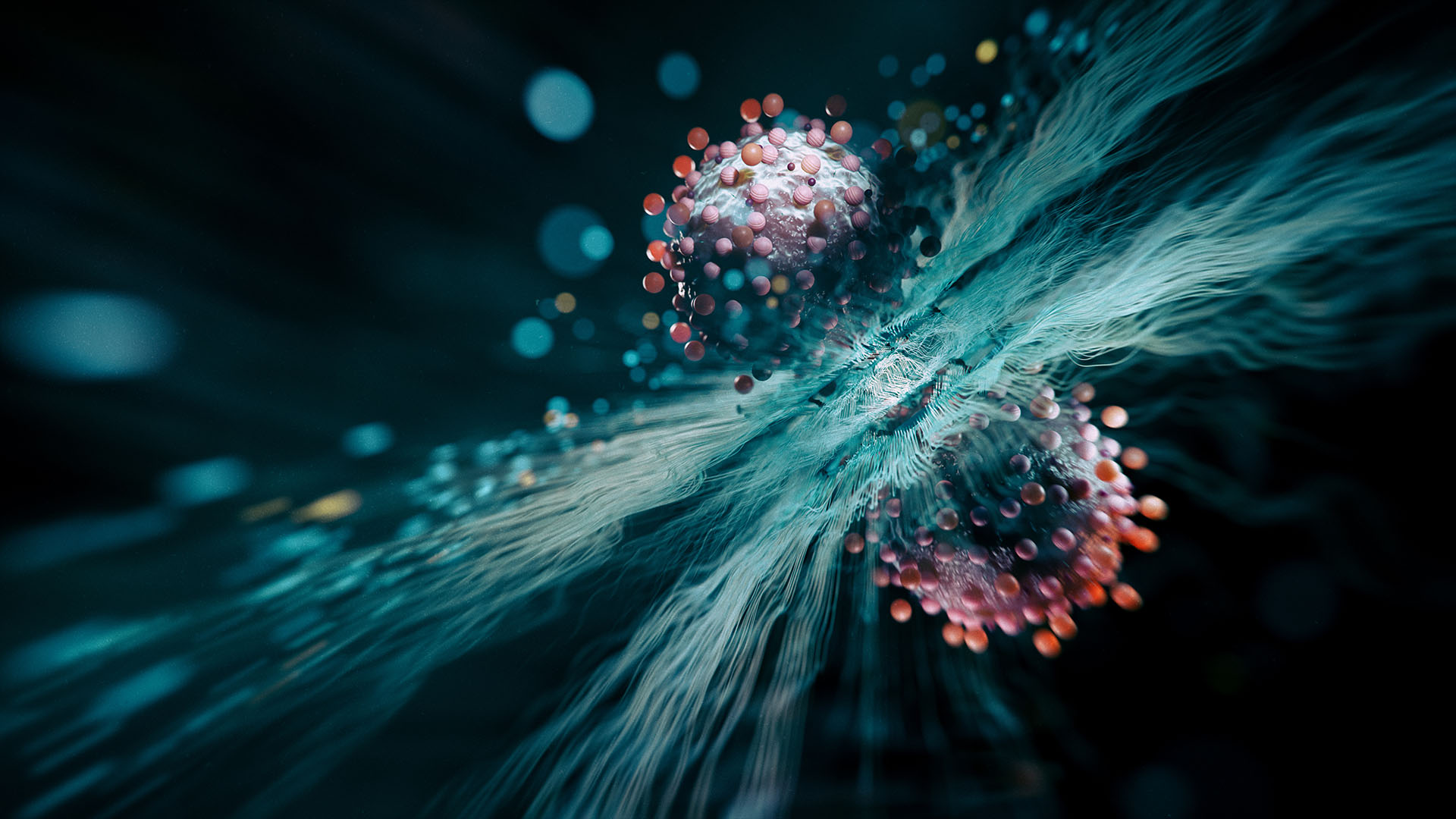
New research I’m presenting today at the annual scientific meeting of the Australasian Society for Infectious Diseases shows that doctors understand the community-wide risks of antibiotic resistance but over-prescribe because they want the best outcomes for individual patients.
The rise of antibiotics – and superbugs
The modern antibiotic era began with the discovery of penicillin in 1928, which led to dramatic improvements in our ability to treat common infections. This was probably the most important discovery in the history of modern medicine. And for a long time, antibiotics reigned supreme in the battle against previously deadly bacterium.
The dramatic improvements of the 20th century, however, are now being undone by overuse and misuse of antibiotics.

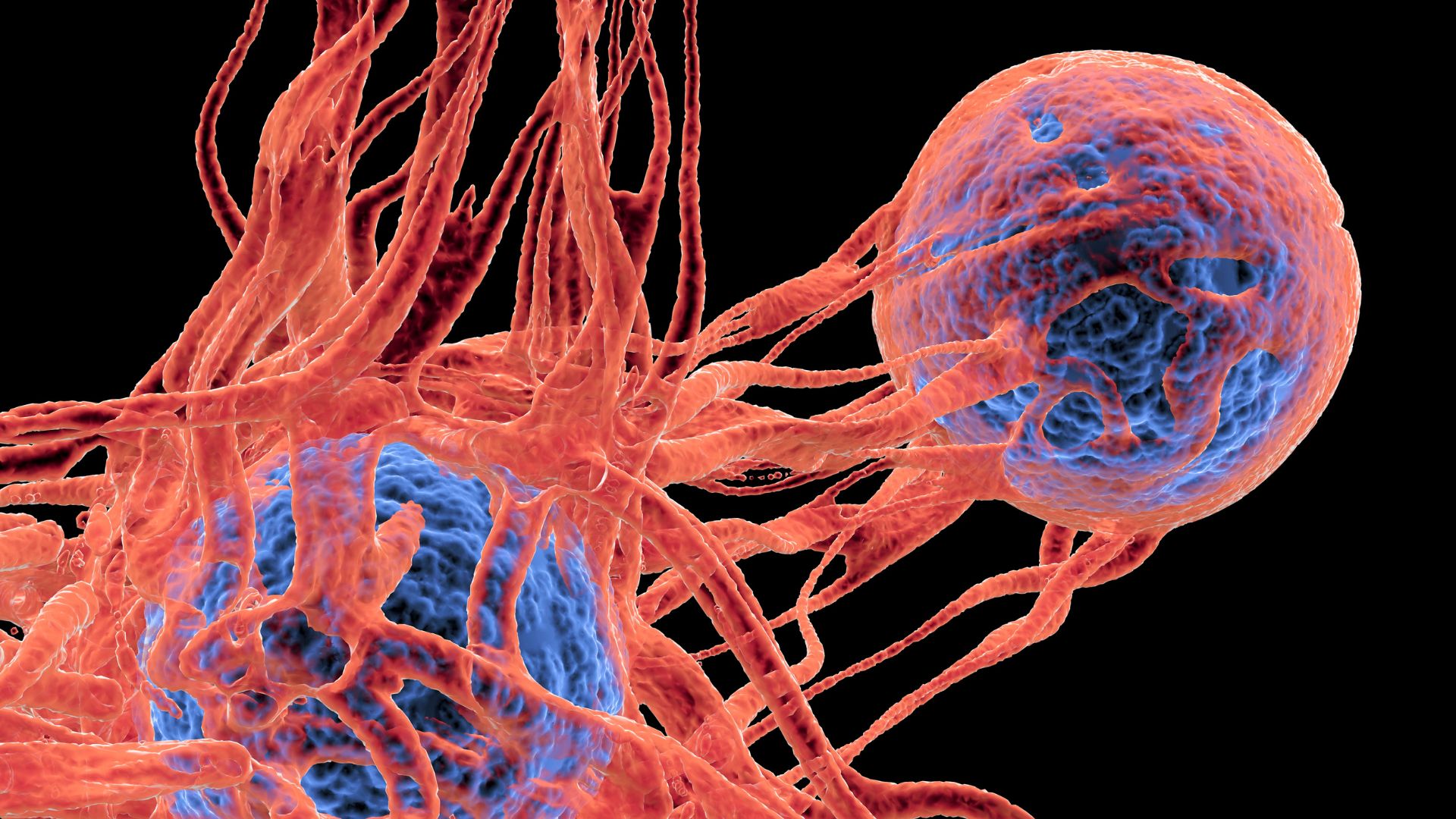
Major resistant organisms including multi-resistant gram negative bacilli (MRGNB), methicillin-resistant Staphylococcus aureus (MRSA) and Vancomycin resistant Enterococci (VRE) are already present in Australia, and for some bacteria, there are literally no treatment options available. Patient survival in such cases is consistent with that seen in the pre-antibiotic era.
Resistant superbugs and poor use of antibiotics are together leading us toward an “antimicrobial perfect storm” in the next few decades. This may sound apocalyptic but it’s simple epidemiology: increasing resistance combined with decreasing antibiotic options will worsen to the point where we will have no capacity to treat previously highly treatable infections.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
The “antibiotic pipeline” of drug development, as it is termed, has been extremely limited for some time now, with only five new chemical classes of antibiotics developed since the 1970s. There are now resistance mechanisms identified to each of these classes.
It is now widely recognised that the development of new antibiotics is not a sustainable strategy in the war against resistant bacteria. As outlined by the World Health Organization, among others, our only option is to protect our current antibiotics by judicious use; retaining their integrity for significant infections. The problem is, this is simply not happening.
Over-prescribing
A recent Australian study found that while approximately 40% of hospital in-patients receive antibiotics, nearly half of those are actually unnecessary or sub-optimal.
Hospital-based “antimicrobial stewardship programs” to reduce inappropriate prescribing may prompt initial shifts in behaviour, but research shows doctors quickly return to inappropriate antibiotic use.
To investigate why, my colleagues and I at the University of Queensland and the Sunshine Coast Health and Hospital Service interviewed 30 hospital-based doctors from a range of specialities.

We found that the hospital environment and medical culture inadvertently promote and perpetuate unnecessary use of antibiotics or overuse of the most potent, broad-spectrum antibiotics.
Despite understanding the long-term risks of resistance, doctors are focused almost exclusively on treating the potential infection in front of them, in their individual patient. Long-term risks are not prioritised and the judicious use of antibiotics is not valued.
On night shifts, junior staff reported over-prescribing antibiotics to avoid having to wake a senior doctor and ask for help. They were also worried about the risk of not acting to prevent or treat the infection.
Senior doctors reported an inability to accept the risk that avoiding prescribing the most potent broad spectrum antibiotic might present.
Towards best practice
This problem of short-term cost for long-term gains speaks to a range of dilemmas currently facing humanity including global financial security and environmental protection; while human beings might understand and worry about long-term consequences, they are drawn to respond to day-to-day immediate risks to themselves and others. And doctors are no different.
The medical fraternity is orientated towards their individual patient and is less concerned about the population-level crisis of antibiotic-resistance. But the reality is, when a doctor is treating their patient, they are, in fact, treating future patients and the broader community.
The question, then, becomes what short-term costs can we tolerate to secure our collective long-term health?

The first logical step to reduce over-prescribing is to create the professional and organisational structures that support careful use of antibiotics, particularly potent, broad-spectrum antibiotics which are our only defence against highly resistant bugs.
Reducing the fear of blame, responsibility or even litigation if all potent antibiotic options aren’t utilised is an important professional issue to address. In other words, we must allow doctors to be more judicious without the potential for blow back if things do go wrong.
Finally, it’s time we all recognised that antibiotics are a diminishing resource and they’re not the solution to all our health problems.
Next time I’m faced with an antibiotics script, I’m going to ask my doctor: do I really need this, or should we let nature take its course? I accept that a small risk to me, and perhaps a slightly longer period being ill, is worth it to secure the future of antibiotics.
Alex Broom receives funding from the Australian Research Council
This article was originally published on The Conversation. Read the original article. The views expressed are those of the author and do not necessarily reflect the views of the publisher. This version of the article was originally published on Live Science.