Our Ability to Cope with Food Poisoning Outbreaks Has Not Improved Much in 50 Years

This article was originally published at The Conversation. The publication contributed the article to Live Science's Expert Voices: Op-Ed & Insights.
On May 7 1964 a catering-size can of corned beef from Rosario, Argentina, was opened in a supermarket in central Aberdeen. Half the contents were put on a shelf behind the cold meat counter and the other half went into the window.
The weather was warm. The sun shone on the meat. Corned beef is cooked in the can and should be sterile. But it wasn’t. It had been contaminated after cooking when the can was cooled with untreated water from the River Parana.
Into this river, 66 tons of human feces and 250,000 gallons of urine were discharged every day from Rosario, where typhoid was common. The bacteria in the corned beef in the window grew vigorously.
Toll rising
The first person to fall ill developed symptoms on May 12. Making an initial diagnosis is not easy; it usually starts with a high fever, which can have many causes.
In Aberdeen the first definitive diagnoses were made on May 20. By midnight 12 were in hospital, and until June 13 daily hospitalisations never fell below double figures. The outbreak then fizzled out. At its end 503 had been admitted to hospital with typhoid, 403 with bacteriological confirmation.
Among those affected, there was a significant over-representation of women aged 15 to 25 living in the more prosperous west end of the city. The probable explanation is that a slimming regime incorporating cold meats and salad was popular at the time.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Nobody died from typhoid in the outbreak, thanks to antibiotics, so in that regard it was modern. Its media coverage, by TV, would be recognisable today too. But some aspects of its management were conducted as though World War II was still in progress. The names and addresses of those admitted to hospital were published in the local paper and the end of the outbreak was announced as the “all clear”.
Dr Ian MacQueen, then Aberdeen medical officer of health, took control of the outbreak. Opinion in Aberdeen is still divided about how he handled it. Some say he saved the city, others that his antics verged on the ridiculous.
I belong to the latter camp. MacQueen believed that dramatic statements of risk were necessary to prevent the spread of infection. Thus Aberdeen became in his description the “beleaguered city”, and beef cattle raisers in Paraguay, Kenya and Tanzania suffered economically as importing meat came to be seen as high risk in the initial panic about the source.
MacQueen recommended that nobody should paddle in the sea, and the main thoroughfare, Union Street, was sprayed with disinfectant. There was an obsession with “wave after wave of infections” occurring because of poor personal hygiene.
In truth this was always very improbable. There was no person-to-person spread. All the infections were caused by eating contaminated corned beef or cold meats cut with the same slicer. New cases continued to appear not because the source of infection was still active but because the incubation period – the time between being infected and falling ill – was often long.
The modern picture
Could the kind of events that happened in Aberdeen 50 years ago be repeated? Cans of food are unlikely to be the source nowadays because canning practices are almost certainly better (even if as we saw in the horse meat scandal, the label does not always accurately describe the contents). Typhoid is still common in countries whose drinking water is regularly contaminated with human feces – the 2004/2005 outbreak in Kinshasa affected 42,564 and killed 214.
But an even nastier organism caused the most recent big food-borne outbreak in Europe. Like the Aberdeen outbreak, it started in May and went on until the end of June, and like Aberdeen it also affected women much more commonly than men. But it happened in 2011 in Germany.
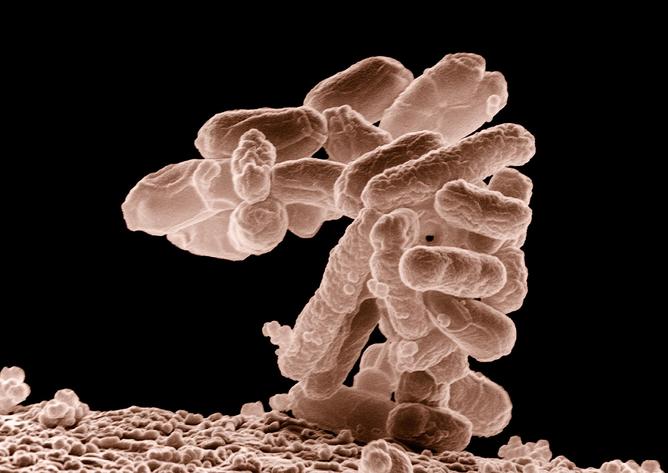
The organism was E.coli O104:H4, a brand-new bacterium that had evolved as a hybrid of two other disease-causing E.coli strains. More than 3500 fell ill, 855 developed serious complications and 53 died.
Just as in Aberdeen, the organism was imported. It came on the surface of fenugreek seeds which had left Egypt by boat on November 24 2009, eventually arriving at an organic sprout producer near Hamburg on February 10 2011.
Seed sprouting is ideal for bacterial growth. But identifying the seed sprouts as the cause of the outbreak was difficult and slow, because were used as a salad garnish and many victims were not aware that they had eaten them. That women were more commonly ill pointed to salads, but photographs taken at meals were invaluable.
It was all very embarrassing for the German public health authorities, particularly when the Hamburg health minister mistakenly announced that the organism that had caused the outbreak had been found on Spanish cucumbers, causing serous economic damage to that industry. Shades of Dr MacQueen!
Lessons from Hamburg
This mistake illustrated the limits of modern lab technology. We might now be in a position where we could genome-sequence E.coli 0104:H4 quickly, but because it was a new strain, the authorities initially confused it for the more prevalent E.coli 0157:H7. When they found this latter bug on the cucumbers, they thought they had found the culprit. New bugs will always make life difficult for scientists.
The German outbreak also pointed to another unavoidable issue: the Egyptians initially denied responsibility. Whatever your technological advances, politics is still likely to slow you down. One bright spot here though is that the Chinese are much more cooperative than they once were. This is vital given that the country’s size and relative concentration of people makes it quite a likely source for outbreaks.
Another important step forward has been global food safety standards. The worldwide adoption of the hazard analysis critical control points system – HACCP – originally developed by NASA to protect astronauts from food poisoning, makes it less likely that the world food supply could lead to a major epidemic – even if some countries are still more diligent than others.
Having said that, food poisoning is more common than a century ago (albeit not dysentry spreading from person-to-person or tuberculosis in milk). The Ministry of Health for England and Wales recorded 59 food poisoning incidents during the years 1931-1935, compared to more than 73,000 in 2012, itself a gross underestimate because most people with food poisoning don’t seek medical advice.
The number of sufferers from the UK’s number one cause, campylobacter, has been convincingly estimated at 500,000 people each year. To some extent this is down to better diagnosis, but probably not entirely. The realities of 21st century mass production of cheap meat are likely to have driven up infection, for example.
Above all else, the big lesson from Germany was that a major outbreak could still take us completely by surprise. With microbes evolving as they do, we can be certain it will happen again.
Hugh Pennington does not work for, consult to, own shares in or receive funding from any company or organisation that would benefit from this article, and has no relevant affiliations.
This article was originally published on The Conversation. Read the original article. Follow all of the Expert Voices issues and debates — and become part of the discussion — on Facebook, Twitter and Google +. The views expressed are those of the author and do not necessarily reflect the views of the publisher. This version of the article was originally published on Live Science.



