Forget Folk Remedies, Medieval Europe Spawned A Golden Age of Medical Theory
This article was originally published at The Conversation. The publication contributed the article to Live Science's Expert Voices: Op-Ed & Insights.
It’s often said that there was no tradition of scientific medicine in medieval times. According to the usual narrative of the history of progress, medicine in the European Middle Ages – from around the 5th to the 15th centuries – was a formless mass of superstition and folk remedies; the very antithesis of science.
And those who look in medieval medicine for precursors of modern pathology, surgery, antibiotics, or genetics will of course find it a failure. But if we’re looking for a coherent medical system that was intellectually and emotionally satisfying to its practitioners and patients, and based on written authorities, rational enquiry, and formal teaching, then medieval Europe produced one of the most influential and scientific medical systems in history.
Medieval medicine did take many forms. Some of it was non-literate and based on inherited traditions, some on the use of simple herbs, while other remedies were based on blaming elves or demons or sin for sickness. Sometimes it was practised by women for their families and servants.
But if we are careful with our definition of “science”, and use it to mean not (as often happens) what we now think is correct but rather a rationally organised body of knowledge about the natural world, then medieval medicine did use scientific methods.
And it was in the 11th century that Europe witnessed a medical revolution. Scholars and physicians in southern Italy, especially in the city of Salerno, began to study and teach ancient medical texts after a hiatus of 500 years or more. We know this from surviving 11th and 12th-century manuscripts that are only now being collectively studied, especially those of a little known medical textbook called the Articella.
The Articella
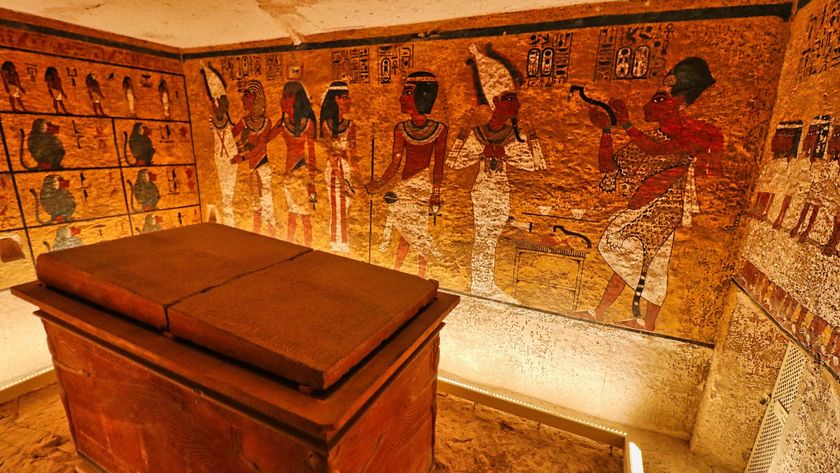
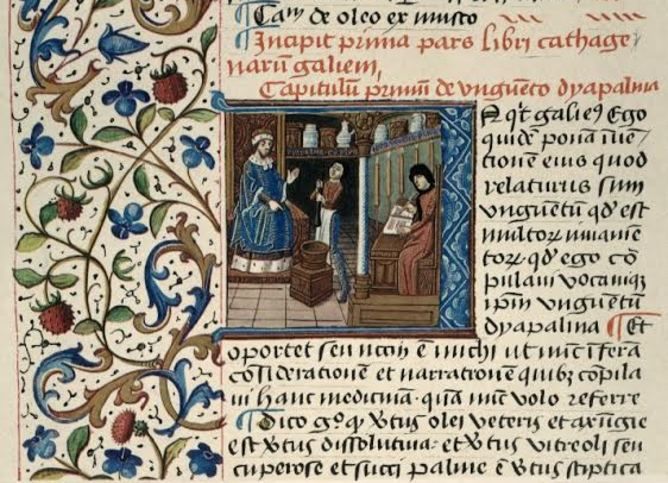
How we view medieval medicine, at the expense of alternate forms, is partly due to the nature of the surviving evidence we have. Apart from rare archaeological finds, this comes mostly from manuscripts primarily from the second half of the Middle Ages (c.1000-1500AD). Many of these manuscripts are copies of medical texts written much earlier, between about 400BC-1000AD. Some of these were in Latin, and had long sat ignored in monastic libraries. Others were in Arabic or Greek and were traded or carried across the Mediterranean to be translated into Latin.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
These texts didn’t just appear; they were actively sought, translated and edited by newly curious medical teachers and practitioners. And they are how we know about a revolution in 11th-century European medicine.
By about 1100AD, an international body of philosophers and physicians, stretching north from Salerno to England, and east from Iberia to the German empire, had organised five Latin texts into a textbook called Ars Medicinae (“The Art of Medicine)” and later nicknamed the Articella (“The Little Art”). The five texts were the Isagoge (or “Introduction”) of Johanittius (an Arab Christian), the Aphorisms and Prognostics of Hippocrates, On Urines by Theophilus, and On Pulses by Philaretus. After about 1150, many copies of the Articella also include Galen’s Tegni (or Ars medica).
This may seem an overwhelming syllabus, but the entire Articella is shorter than any modern medical textbook. Each text served a different function in the classroom. The Isagoge was a brief introduction to medical theory. And through Hippocrates' Aphorisms and Prognostics, students learned brief and useful statements on medical practice by this father of medicine. The Byzantine Greek texts by Theophilus and Philaretus were the most practical, giving instructions for making diagnoses and prognoses with a patient’s urine and pulse. The Tegni encompassed and surpassed the first five texts, and so served as the basis of university exams and commentaries for centuries to come.
By 1200 the Articella was accepted throughout Europe as the foundation of medical education. Medieval university faculties of medicine made the Articella required reading along with the Canon of Medicine by Avicenna, first translated into Latin in the 1170s.
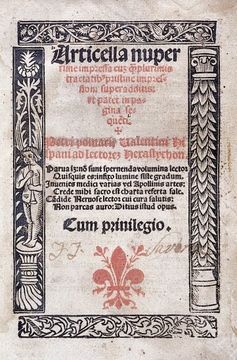
And after the invention of printing, the book appeared in at least 16 editions to 1534, surviving well beyond the usual dates for the Middle Ages.
It’s obvious that the Articella was popular, but why does it matter so much? The vast number of healers, men and women, had never read it. But the widespread acceptance of the Articella set the bar for medicine across Europe.
Every doctor, especially itinerant male healers in search of a wide clientele, had to know (or at least pretend to know) the rational medicine taught in the schools.
Knowledge of this distinctly medieval medicine, which was built on Greek and Arabic foundations but developed by generations of medical teachers and students into something new, was expected of any proper physician. Even those not directly involved in medicine, such as philosophers, lawyers, and theologians, began to incorporate learned medicine into their writings.
Corruption of the humours
By the 12th century and up to the 16th, the majority of people in the noble, mercantile, and clerical classes of European cities agreed on a specific form of medical learning, generally known as scholastic medicine. Ideally, this medicine was practised only by Christian men and written in Latin. It was a highly literate science that was taught in the universities, and was based on the writings of ancient Greek and medieval Arabic physicians, especially Hippocrates (5th century BC), Galen (c.130-200AD), and Avicenna (the Latinised name of Ibn Sina, 980-1037AD) – one of the foremost thinkers in the Islamic world.
These authors and their medieval Latin followers created a medicine that was thoroughly holistic: sickness was explained by the imbalance or corruption of the four humours (blood, phlegm, yellow bile, black bile), the four principal liquids of the body. And health was achieved by the balance and proper cultivation of the humours. Each was necessary to human nature, but each could also grow too abundant or corrupted.
Physicians used these humours to explain every complaint – medical or psychological. The dominant pattern or mixture of humours determined a person’s complexion, a term referring not to the skin but to one’s entire bodily and mental constitution. And everyone’s complexion was slightly different, especially between the sexes, and also changed as one aged.
A physician’s course of treatment had to be tailored to the individual patient, or at least to their age group and gender. Diagnosis and prognosis took into consideration the whole person – using a system developed by Arab physicians out of Galen’s writings and called the “six non-naturals” – by which the physician ideally examined his patient’s food and drink, air and environment, sleep and wakefulness, motion and rest, evacuation and repletion, and emotions.
So before undertaking treatment, a physician trained in Galenic medicine took into consideration a wide range of factors, including complexion, environmental and personal “non-naturals”, and symptoms of the disease.
By the end of the Middle Ages, an educated physician might also look to the stars and cast horoscopes of his patient to determine prognosis and course of action. And treatments were generally conservative, tending toward advice on diet, exercise or bathing. When medicines were prescribed they were based on local herbs and alcohol for the average client or exotic spices and sugar for the wealthy – the former available from any village herbalist and the latter from apothecaries in urban areas.
Placebo action
Most of the regimens and prescriptions in surviving manuscripts would not have cured any condition, apart from improving the patient’s mood, but neither would they have done any harm. If their condition improved, credit could be given to the physician. If their did not improve, blame could be applied to anyone from the patient, the spouse, or children, or servants, the physician, or even the apothecary.
Therein lies part of the durability of medieval medicine: it offered a satisfactory explanatory system for disease in the absence of anything better, and the physician was not expected to work wonders, since he bore only part of the responsibility for treatment and cure.
The science of medieval medicine was centuries in the making: Arab physicians and teachers of the 10th to the 12th centuries, and Latin ones after the 11th worked and reworked the complicated inheritance of ancient medicine into a convenient, flexible, and rational system.
Despite its failure (by modern standards) to identify or cure most diseases, the medieval medicine of the Articella satisfied patients and practitioners for half a millennium, surviving even the Black Death and the Renaissance, to last well into the early modern era.
Winston Black does not work for, consult to, own shares in or receive funding from any company or organisation that would benefit from this article, and has no relevant affiliations.
This article was originally published on The Conversation. Read the original article. Follow all of the Expert Voices issues and debates — and become part of the discussion — on Facebook, Twitter and Google +. The views expressed are those of the author and do not necessarily reflect the views of the publisher. This version of the article was originally published on Live Science.
Winston Black is a historian of medicine and religion in medieval Europe, and has taught at numerous universities in the United States and Canada. His research focuses on medieval pharmacy (drugs, herbs, and spices) and the interactions between medicine and theology in the High Middle Ages. His publications include "Medicine and Healing in the Premodern West: A History in Documents," (Broadview Press, 2019), "The Middle Ages: Facts and Fictions" (ABC-CLIO, 2019) and "A History of the Middle Ages, 300-1500, Second Edition (2016)" (Rowman & Littlefield Publishers, 2016).