What is a fecal transplant?
Fecal transplants have become a common procedure to treat bowel infections – but how do they work and are there any risks involved?

Fecal transplants are a relatively new area of medicine often used to treat bowel infections, particularly clostridium difficile, a nasty, sometimes life-threatening infection that can occur after a course of antibiotics. C. difficile can cause serious inflammation in the bowel, which leads to symptoms such as abdominal pain, cramping and diarrhea – as well as general symptoms of an infection, including fever and nausea. Dehydration is also a risk with this infection, as a lot of water is passed through diarrhea.
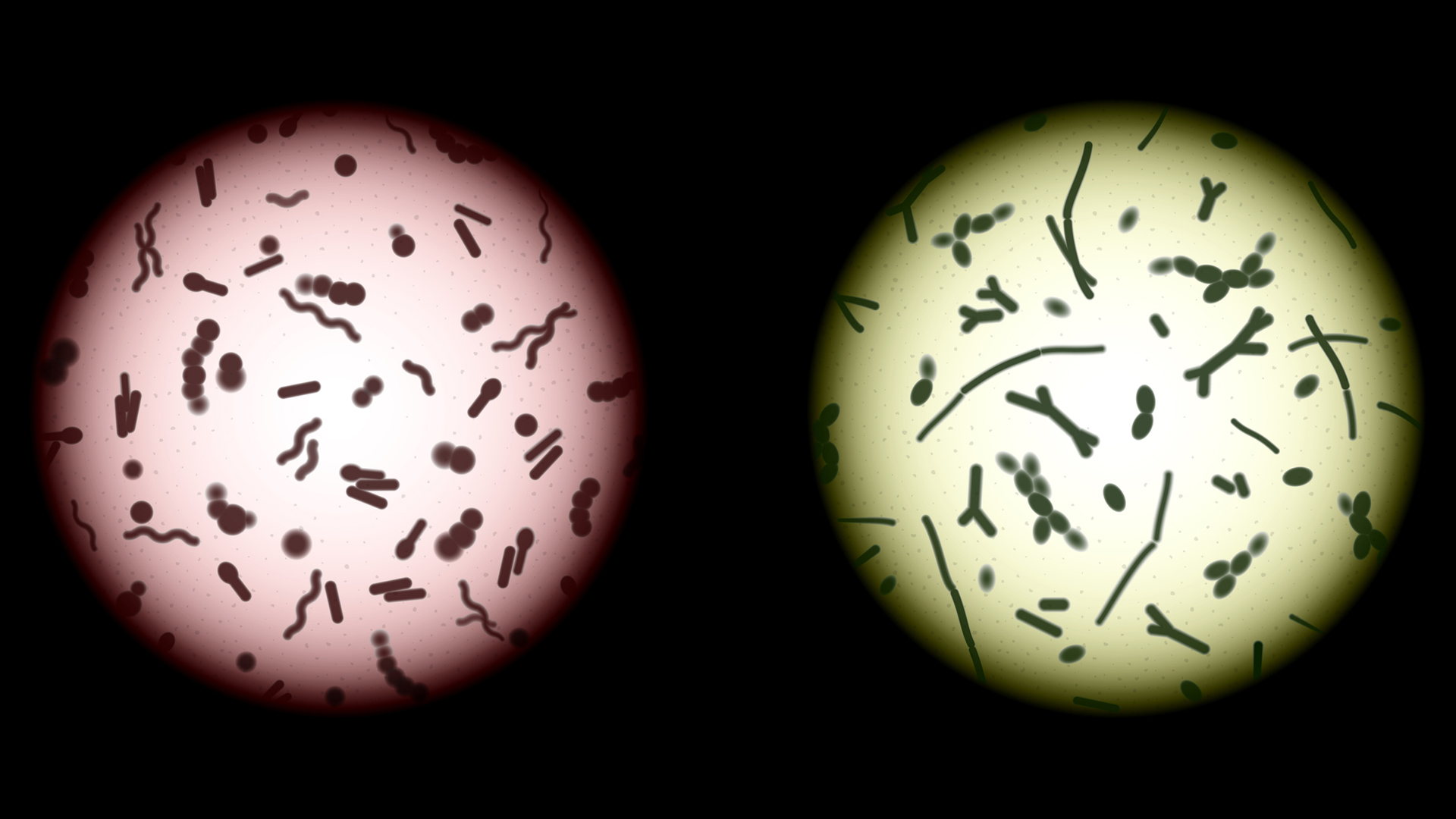
So what is a fecal transplant? It is exactly what it sounds like: a healthy donor provides a stool sample, which is then transplanted into the infected person in an attempt to help their gut flora to bounce back and repopulate after a clostridium difficile infection.
Our gut microbiome plays a large part in our overall immune health, as well as being linked with mental health through the gut-brain axis, so gut health has never been more important. Read on to discover the ins and outs of fecal transplants.
What is a fecal transplant?
Dr Duane Mellor, lead for nutrition and evidence-based medicine at Aston University, outlines the process of fecal transplantation. “As the feces or stool is a biologically active complex mixture of living organisms it has long been thought to have therapeutic potential,” he says. “A fecal transfer from healthy donors, often to someone with a bowel infection, is to try and replace disease-causing bacteria with ones that may be beneficial.”

Duane Mellor is a registered dietitian and lead for Nutrition and Evidence Based Medicine at Aston Medical School. Having a background in clinical dietetics supporting people living with diabetes, he moved into medical education when joining Aston University. He is also the Associate Dean for Education (Quality Enhancement) in the College of Health and Life Sciences.
According to Mellor, it was first used in fourth-century China, where Ge Hong described the use of human fecal suspension by mouth for patients with food poisoning or severe diarrhea – not that we would ‘feed’ people this way now.
“It is used to treat conditions like pseudomembranous colitis, which has been treated by fecal enemas since 1985,” he adds. “Typically, it is given via a tube into the intestine, which can be to the end of the first part of the small intestine via an endoscopy or by a colonoscopy into the first part of the colon, as it is important that the transplant can be distributed throughout the whole colon, as this is the area where most of the microbes in our gastrointestinal tract are found.”
A review in the Journal of the Formosan Medical Association indicates that while fecal transplantation is considered a generally safe therapeutic method with few adverse effects, (approved by the FDA for treatment of C difficile infection in 2013), the long-term outcomes are not certain. Once the research catches up, hopefully we will have a clearer idea of the long-term impacts of fecal transplants.
“The donors are typically young (10-25 year olds) and have not taken antibiotics, laxatives or diet pills, which can all change the bacteria found in the colon and feces,” adds Mellor. “They must also be free from any gastrointestinal disease and will be screened for inflammation and infections, including hepatitis and HIV. The donated stool needs to be transplanted or stored within one hour. Prior to transplanting, it is centrifuged, filtered and diluted.”
A study in the Journal of Clinical Gastroenterology testing the efficacy of fecal transplants on 146 elderly patients showed promising results. C. difficile is particularly dangerous for the elderly, with a higher chance of morbidity than other age groups. Unfortunately, during the test one patient experienced an adverse event of CDI-related diarrhea that resulted in their death. However, overall results indicated that primary and secondary cure rates were 82.9% and 95.9% respectively, and early and late recurrences occurred in 25 and six patients respectively, which is overarchingly positive.

Dr Deborah Lee, MD at Dr Fox Online Pharmacy, explains why someone may contract clostridium difficile, which can be a serious and difficult-to-treat condition.
“C.difficile is a bacterium that is normally found in the bowel,” she says. “However, taking a course of antibiotics can upset the balance of bacteria that inhabit the small and large intestines. These ‘good’ bacteria help to keep levels of C.difficile in check. When the number of good bacteria is reduced, C.difficile can multiply. It produces an endotoxin that causes inflammation in the bowel wall, abdominal pain, and profuse, watery diarrhea.”

Having worked for many years in the U.K's NHS, initially as a GP, and then as Lead Clinician for an integrated Community Sexual Health Service, Dr Deborah Lee now works as a health and medical writer, with an emphasis on women’s health. She is a menopause specialist. Dr Lee is a medical content writer for Dr Fox.
She adds that C.difficile can also be passed from person to person through touching contaminated hands or acquired from contact with infected work surfaces. It can be present in water, soil, and may be present in raw meat.
“Fecal transplant is a possible new cure for those with severe, persistent, or recurrent C.difficile infection, for whom effective management can be challenging,” says Lee.
What's the science behind fecal transplants?
Although somewhat unconventional, fecal transplants can be effective, particularly in treating complex and severe C. difficile infections. Mellor explains: “It has been seen to be associated with up to 90% resolution of diarrhea following clostridium difficile infection with studies reporting no adverse side effects, this compares to around 30% treated with the antibiotic vancomycin.
“There are reports, largely as cases which may not provide such robust evidence for people with inflammatory bowel disease, with up to 70% resolution of IBD symptoms and reduction/cessation of IBD medications within six weeks, and specifically in Crohn’s disease a clinical remission in 50% of patients. These findings seem positive but we need more robust data to be sure that these effects are reproducible.”
He also says that there is some evidence that sterile fecal transplants may help with clostridium difficile infection, suggesting it might not be the viable bacteria and bacteriophages (viruses that infect bacteria and may also be helpful), but the proteins and other material that come in a fecal transplant.
Additionally, fecal transplantation may offer effective support for antibiotic treatments, which can be ineffective when used alone. A study in the New England Journal of Medicine indicates that C. difficile infection recurred in 31% of patients who received only the antibiotic vancomycin without also receiving fecal transplant. Those who had donor-feces infusions showed increased fecal biodiversity, at similar levels to those of the healthy donors.
Fecal transplant: Are there any risks?
As with all medical procedures, there is a degree of risk associated with fecal transplantation. Mellor says that fecal transplants should be undertaken with caution.
“The risks may be for those who are immunocompromised, as even what are thought to be friendly bacteria, can lead to infection. So, in these individuals the emerging evidence for sterile transplants is of interest.” he says.
There has been at least one case of death, where a drug resistant bacteria was transplanted and led to an infection that could not be treated. According to Mellor, it is essential that transplants are properly screened and checked as there are risks of infection if this is not done adequately.
Lee explains that the prerequisites for a donor sample are carefully considered, to keep the risk of infection as low as possible. “The feces must come from a donor who has not had antibiotics for at least six months and has tested negative for infections such as HIV, hepatitis B and C, norovirus, Epstein-Barr virus, and cytomegalovirus,” she says. “This is especially important if the transplant is for an immunocompromised patient. There is concern about the possible transmission of Covid-19 via this transplantation, and donated fecal samples are also tested for the presence of the virus.”
Other possible negative side effects include:
- After the procedure there may be side effects, such as bloating, belching, nausea, diarrhea, and abdominal pain.
- Other bacterial pathogens may be transferred in the donor feces, such as beta-lactamase producing E.coli, which has led to one death.
- The route of administration is also a risk. In one study, 43.9% of patients undergoing transplantation who had had it inserted via upper GI endoscopy, reported adverse events, as opposed to 20.6% who had it inserted by colonoscopy.
- Bowel perforation is a rare complication of a colonoscopy, which can be fatal.
- Inserting the donor faces via a nasogastric tube has led to aspiration pneumonia.
- Possible long-term adverse effects of receiving donor bacteria – whether this could increase the risk of autoimmune diseases or conditions, such as obesity in the future, are not known.
This article is for informational purposes only and is not meant to offer medical advice.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.

Lou Mudge is a health writer based in Bath, United Kingdom for Future PLC. She holds an undergraduate degree in creative writing from Bath Spa University, and her work has appeared in Live Science, Tom's Guide, Fit & Well, Coach, T3, and Tech Radar, among others. She regularly writes about health and fitness-related topics such as air quality, gut health, diet and nutrition and the impacts these things have on our lives.
She has worked for the University of Bath on a chemistry research project and produced a short book in collaboration with the department of education at Bath Spa University.










