Combatting TBI by Engineering Resilience in the Brain
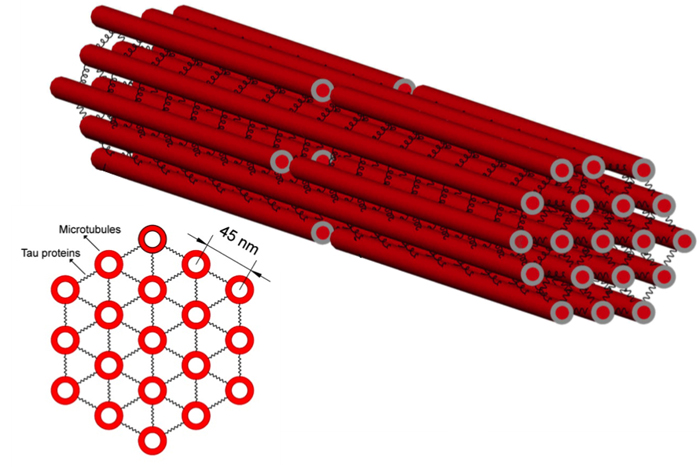
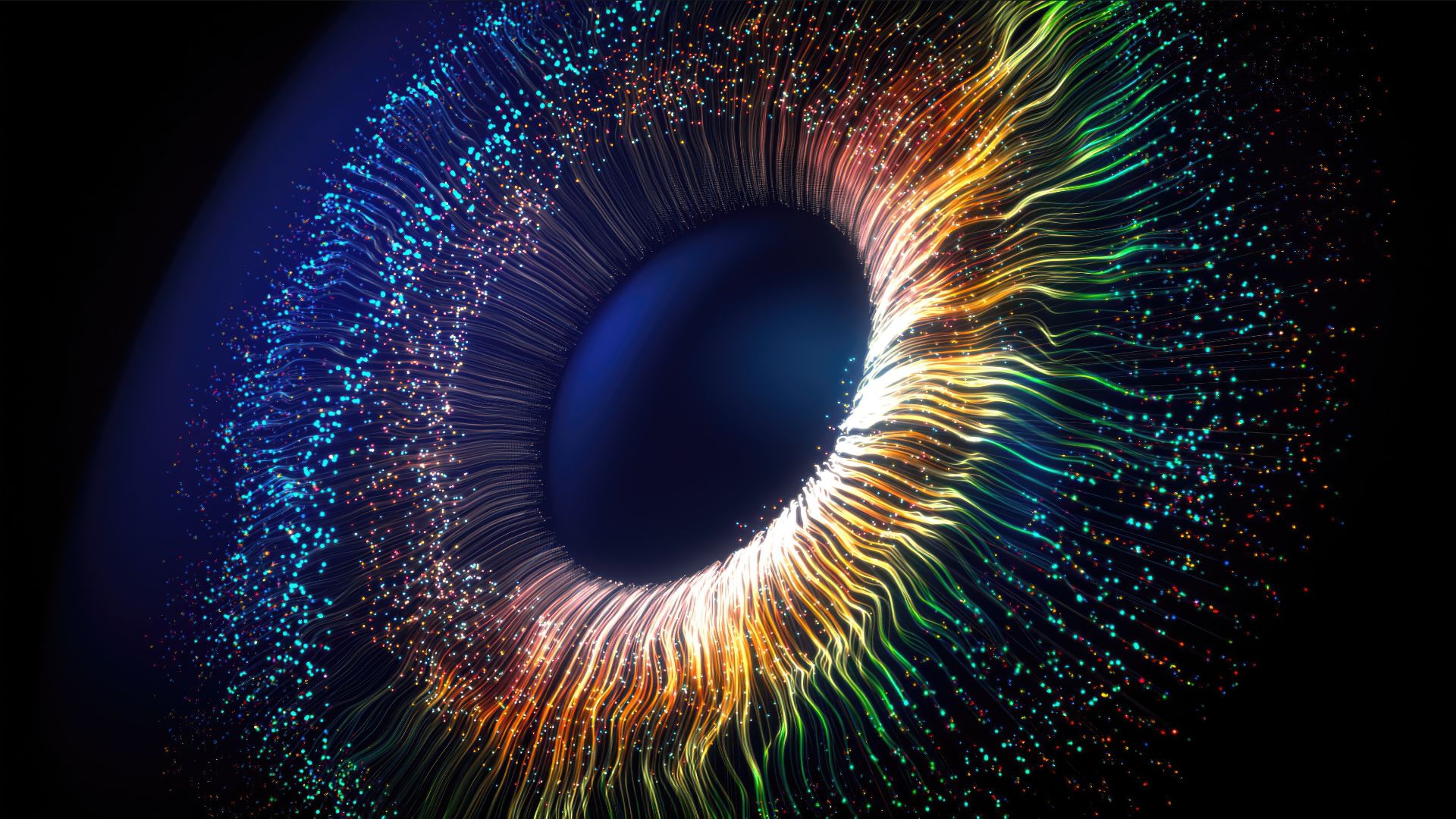
New computational modeling research shows that with sudden strain, like that caused by certain head injuries, tau is less able to stretch and absorb the stress. This stress is thus passed to the microtubules, which break. The result: accumulations of molecular cargo, which are one of the major signs of a traumatic brain injury. (Image credit: University of Pennsylvania )
This Behind the Scenes article was provided to Live Science in partnership with the National Science Foundation.
Compared to the monumental machines of science, such as the International Space Station or the Large Hadron Collider , the human brain doesn't look like much. However, this three-pound amalgam of squishy cells is one of the most complicated and complex structures in the known universe.
Understanding the fundamental wiring of the brain, with its hundreds of billions of neurons, each with an inner world of organelles and molecular components, is a major undertaking — one that has received a commitment of at least $100 million worth of federal funding from the National Science Foundation (NSF), the National Institutes of Health and the Defense Advanced Research Projects Agency.
Protecting or repairing this complicated machine and all of its interconnected structures means thinking like an engineer.
"The idea is really quite simple," says Vivek Shenoy, an NSF-supported professor of materials science and engineering at the University of Pennsylvania's School of Engineering and Applied Science. "All of the mechanical properties of cells come from their cytoskeleton and the molecules within it. They're all reinforcing frames, like the frame in a building. Engineers design buildings and other structural objects to make sure they don't fail, so it's the same principle: structural engineering on a very, very small level."
Shenoy applies this approach to a problem very much in the public eye — traumatic brain injury (TBI). Even the mildest forms of TBI, better known as concussions, can do irreversible damage to the brain. More serious forms can be fatal. [Concussions Deal Bigger Blow to Men Than Women ]
Shenoy has a background in mechanical engineering and materials science, but his method for addressing TBIs does not involve designing new helmets or other safety devices. Instead, he and his colleagues are uncovering the fundamental math and physics behind one of the core mechanisms of the injury: swelling in axons (the tendril-like offshoots of neurons) caused by damage to internal structures known as microtubules. These neural "train tracks" transport molecular cargo from one end of a neuron to another; when the tracks break, the cargo piles up and produces bulges in the axons that are the hallmark of fatal TBIs.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Armed with a better understanding of the mechanical properties of these critical structures, Shenoy and his colleagues are laying the foundations for drugs that could one day bolster neurons' reinforcing frames, increasing their resilience to a TBI-inducing impact.
Train Tracks and Crossties
The first step toward achieving this improved understanding of neural "train tracks" was resolving a paradox: why were the microtubules, the stiffest elements of the axons, the parts that were breaking when loaded with the stress of a blow to the head?
Shenoy's team showed that the answer rests with a critical brain protein known as tau, which is implicated is several neurodegenerative diseases, including Alzheimer's. If microtubules are like train tracks, tau proteins are the crossties that hold them together. The protein's elastic properties help explain why rapid movement of the brain, whether on a football field or a car crash, lead to TBI.
Shenoy's colleague Douglas Smith, professor of neurosurgery in Penn's Perelman School of Medicine and director of the Penn Center for Brain Injury and Repair, had previously studied the mechanical properties of axons, subjecting them to strains of different forces and speeds.
"What we saw is that with slow loading rates, axons can stretch up to at least 100 percent with no signs of damage," Smith said. "But at faster rates, axons start displaying the same swellings you see in the TBI patients. This process occurs even with relatively short stretches at fast rates."
To explain this rate-dependent response, Shenoy and Smith had to delve deeper inside the structure of microtubules. Building on Smith's work, other biophysical modelers had previously accounted for the geometry and elastic properties of the axon during a stretching injury, but they did not have good data for representing tau's role.
"You need to know the elastic properties of tau," Shenoy said, "because when you load the microtubules with stress, you load the tau as well. How these two parts distribute the stress between them is going to have major impact on the system as a whole."
Elastic Properties
Shenoy and his colleagues had a sense of tau's elastic properties but did not have hard numbers until 2011, when a Swiss and German research team physically stretched out lengths of tau, plucking it with the tip of an atomic force microscope.
"This experiment demonstrated that tau is viscoelastic," Shenoy said. "Like Silly Putty, when you add stress to it slowly, it stretches a lot. But if you add stress to it rapidly, like in an impact, it breaks."
This behavior is caused by the arrangement of the strands of tau protein: they are coiled up and bonded to themselves in different places. Pulled slowly, those bonds can come undone, lengthening the strand without breaking it.
"The damage in traumatic brain injury occurs when the microtubules stretch but the tau doesn't, as they can't stretch as far," Shenoy said. "If you're in a situation where the tau doesn't stretch, such as what happens in fast strain rates, then all the strain will transfer to the microtubules and cause them to break."
With a comprehensive model of the tau-microtubule system, the researchers were able to boil down the outcome of rapid stress loading to equations with only a handful of variables. This mathematical understanding allowed the researchers to produce a phase diagram that shows the dividing line between strain rates that leave permanent damage versus ones that are safe and reversible.
Next Steps
Deriving this mathematical understanding of the interplay between tau and microtubules is only the beginning.
"Predicting what kind of impacts will cause these strain rates is still a complicated problem," Shenoy said. "I might be able to measure the force of the impact when it hits someone's head, but that force then has to make its way down to the axons, which depends on a lot of different things.
"You need a multiscale model, and our work will be an input to those models on the smallest scale."
In the longer term, identifying the parameters that lead to irreversible damage could lead to a better understanding of brain injuries and diseases and to new preventive measures. Eventually, it may even be possible to design drugs that alter microtubule stability and the elasticity of axons that have been involved in a traumatic brain injury; Smith's group has already demonstrated that treatment with the microtubule-stabilizing drug taxol reduced the extent of axon swellings and degeneration after injuries in which they are stretched.
Ultimately, insights on the molecular level will contribute to a more comprehensive view of the brain and its many hierarchies of organizations.
"When you're talking about something's mechanical properties, stiffness is what comes to mind," Shenoy said. "Biochemistry is what determines that stiffness in the brain's structures, but that's only at the molecular level. Once you build it up and formulate things at the appropriate scale, protecting the brain becomes more of a structural engineering problem."
Editor's Note: The researchers depicted in Behind the Scenes articles have been supported by the National Science Foundation, the federal agency charged with funding basic research and education across all fields of science and engineering. Any opinions, findings, and conclusions or recommendations expressed in this material are those of the author and do not necessarily reflect the views of the National Science Foundation. See the Behind the Scenes Archive.