Health Check: What You Should Know About Varicose Veins

This article was originally published at The Conversation. The publication contributed the article to Live Science's Expert Voices: Op-Ed & Insights.
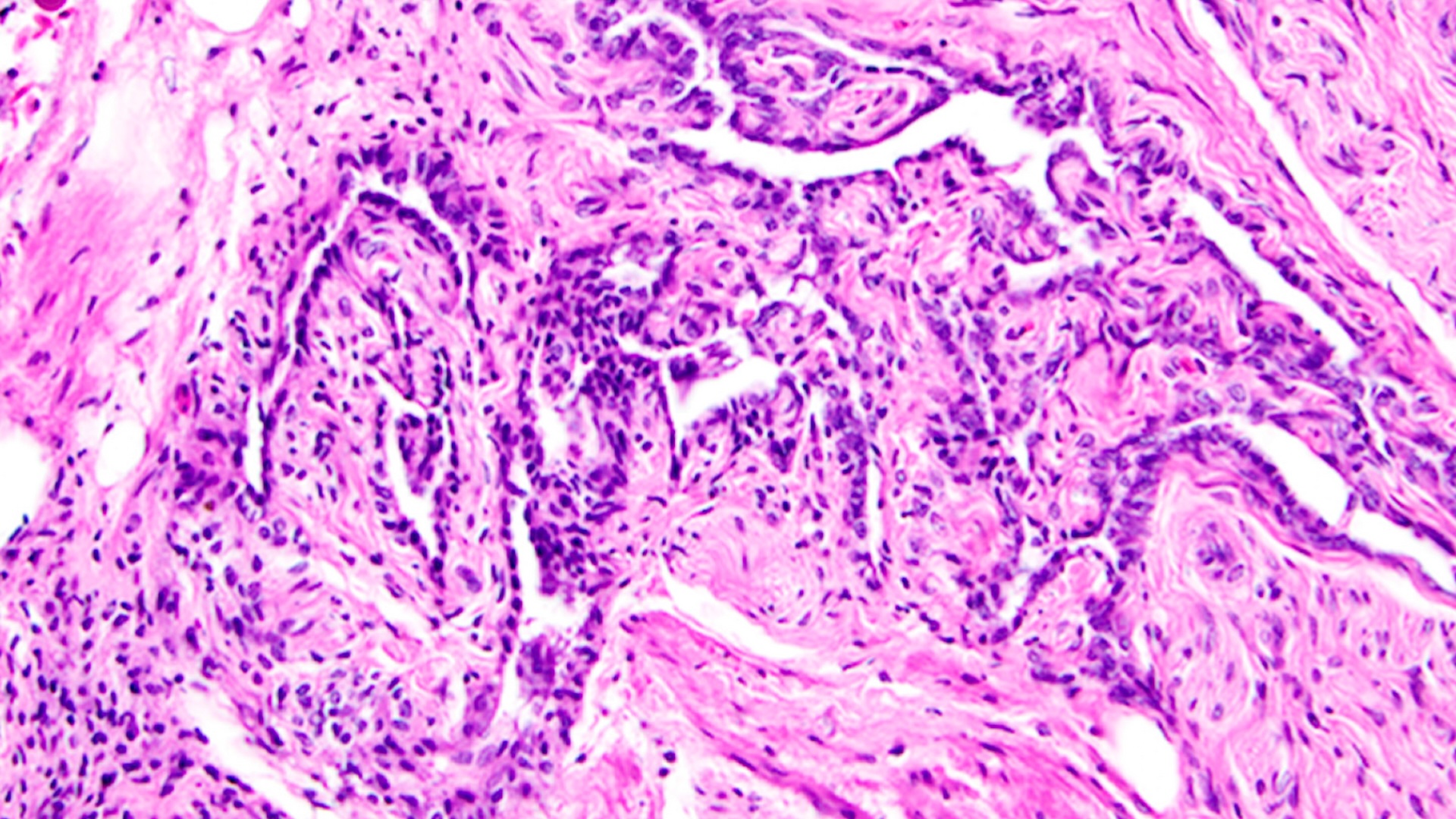
Veins are part of the body’s extensive network of blood vessels, returning blood back to the heart to maintain a continuous circulation. And when things go wrong with them, you can end up with varicose veins.
The heart and blood vessels are known collectively as the circulatory system. With each heartbeat, oxygen-rich blood is pumped through arteries to all parts of the body. Tiny capillaries in body tissues allow the oxygen to be released, for use by cells.
Veins transport de-oxygenated blood back to the heart, ready to be pumped to the lungs to receive more oxygen. As they transport blood against the force of gravity, veins require special mechanisms to ensure that blood doesn’t flow backwards.
Deep and not so deep
There are two types of veins. Superficial veins are the ones you see as blue or purple vessels just under the skin. They have one-way valves to keep blood moving in the correct direction – towards the heart.
Deep veins lie between large muscles in the legs and arms. These veins don’t have valves and rely on the pumping action of the surrounding muscles to keep the blood moving. When you’re walking, for instance, muscle activity compresses the veins in your feet and legs.
These important mechanisms to assist blood flow through the veins are referred to as the “calf muscle pump” and the “foot pump”.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
If the valves in the superficial veins don’t function efficiently, blood can flow backwards (this is known as venous reflux). This causes the pressure inside the vein to increase, leading to venous hypertension.
The thin walls of veins are not capable of withstanding much increase in pressure and they get pushed outwards. It’s these distended and visible veins that are known as varicose veins - “swollen, twisted, lengthened” veins.
Increased pressure inside varicose veins can also dilate much smaller veins, commonly around the ankles. These are known as spider veins (telangiectasias), but they are not, in fact, veins at all. They’re actually dilated capillaries that are less than one millimetre in diameter.
Causes and prevalence
Varicose veins occur most commonly in the legs and thighs. Someone with varicose veins may become very self conscious about the appearance of their legs, but these distended veins can also cause pain, itching, aching and tired legs, muscle cramps and swollen ankles.
Indeed, they may have a negative effect on a person’s quality of life and have been associated with depression.
Visible varicose veins in the legs affect at least one third of the population and become more common with age. Women are more likely than men to develop them and all people with a family history of venous disease are at increased risk.

There’s also a strong link between obesity and varicose veins, especially for women.
Varicose veins often develop during pregnancy, due to a combination of factors including increased hormone levels, increased elasticity of the tissues, and increased blood volume.
In later pregnancy, compression of veins in the groin by the growing baby has an impact. And women who have more than two pregnancies are at greater risk.
Other risk factors
Standing or sitting for long periods of time increases gravitational force on the legs and is another risk factor. And people who’ve had a deep vein thrombosis (blood clot in the deep leg veins) are very likely to develop varicose veins as part of what is knows as “post-thrombotic syndrome”.
High-heeled shoes are known to change muscle function in the leg and have been incorrectly proposed as a cause of varicose veins. Calf muscle activity is actually increased when walking in high-heeled shoes and this decreases pressure in the leg veins.
Varicose veins can lead to more serious problems and it’s important to seek advice from a general practitioner or hospital doctor in the event of bleeding varicose veins, skin changes in the leg, a suspected blood clot (thrombosis), or a break in the skin that will not heal (ulceration).
Still, they’re not always problematic but if you’re at risk of developing varicose veins, here are some suggestions to reduce that chance.
Preventing varicose veins
• Walk regularly to improve circulation of blood in your legs and reduce pressure inside the veins.
• Do foot and leg exercises if sitting for long periods of time. Raise your heels to shift pressure on to your toes for instance, or rotate your feet and ankles to aid circulation in the legs.
• Avoid standing without moving, as the leg muscles aid circulation of blood in the legs.
• Put your feet up when sitting to reduce pressure inside leg veins and minimise ankle swelling.
• Consider wearing light compression full-length socks or tights, as these reduce the pressure inside veins and can improve aching legs. A nurse specialist or a general practitioner can prescribe graduated compression stockings for more severe varicose veins.
• Maintain a healthy weight as obesity increases pressure inside the leg veins.
• Eat a healthy diet including high-fibre foods because constipation and straining during bowel movements can worsen varicose veins.
Caroline Robinson does not work for, consult to, own shares in or receive funding from any company or organisation that would benefit from this article, and has no relevant affiliations.
This article was originally published on The Conversation. Read the original article. Follow all of the Expert Voices issues and debates — and become part of the discussion — on Facebook, Twitter and Google +. The views expressed are those of the author and do not necessarily reflect the views of the publisher. This version of the article was originally published on Live Science.