Best Birth Control for Teens: Implants, IUDs

For teens, the first choice for birth control should be the long-acting forms of birth control, such as intrauterine devices and progestin implants, according to new guidelines from the American Academy of Pediatrics (AAP).
Once implanted in a teen's body, these devices prevent pregnancy for years; they are referred to as long-acting reversible contraceptives (LARC). The new guidelines update a 2007 policy statement from the AAP that emphasized abstinence and condom use.
"What has happened in the past 10 years is that there have been increasing data supporting the safety and efficacy of LARC use in teenagers and adolescents," said Dr. Mary Ott, an associate professor of pediatrics at the Indiana University School of Medicine in Indianapolis and one of the lead authors of the new guidelines. "The policy statement reflects that increase in safety and effectiveness."
The American College of Obstetricians and Gynecologists and the Centers for Disease Control and Prevention have already backed long-acting birth control as the preferred contraceptive method for adolescents and teens. The use of intrauterine devices (IUDs) and implants remains low among young women; data from 2006-2010 found that 4.5 percent of 15- to 19-year-olds used one of these forms of birth control. However, use has increased over the past decade, according to the AAP.
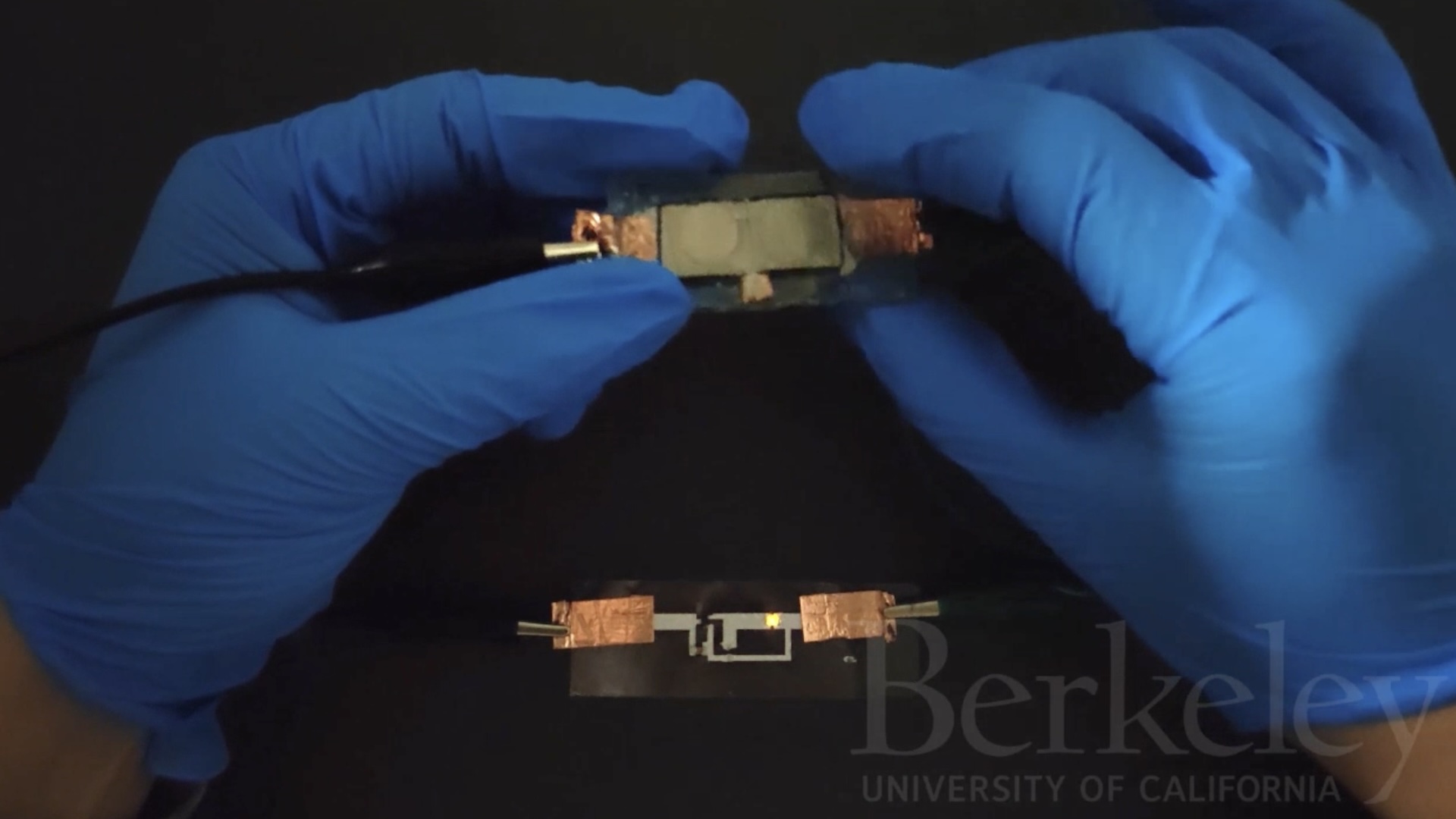
Progestin implants are flexible rods about the size of a matchstick that are placed under the skin of the upper arm, and remain effective for three years after implantation. The brands Implanon and Nexplanon are available in the United States. [Birth Control Quiz: Test Your Contraception Knowledge]
The three IUD brands now available in the United States are the copper-containing ParaGuard, and Mirena and Skyla, which release the hormone levonorgestrel. ParaGuard is approved for up to 10 years of use, Mirena for five years and Skyla for three years.
IUDs have gotten a bad rap, largely due to the decades-old case of the Dalkon Shield, which was pulled off the market in the 1970s after women who used the device developed pelvic infections, Ott said. However, she added, there are now 20 years' worth of data backing the safety and effectiveness of today's copper and levonorgestrel IUDs.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Two of the biggest barriers to LARC use among young people are cost and access, Ott said. But when these barriers are removed, most women — and more than half of adolescents — will chose an implant or IUD over other forms of birth control, she said.
Parents may also be concerned about the safety of these methods for their teens, she added. "I will often times remind them that all contraceptive methods are medicines and devices, and they all have side effects, and that the current LARCs are all safer than pregnancy."
The more widely used contraceptive methods such as the birth control pill, condoms and the diaphragm, have one big problem: The rates of women who continue to use them after starting are low, said Dr. Ann Davis, a clinical professor of obstetrics, gynecology and pediatrics at the Geisel School of Medicine at Dartmouth in Hanover, New Hampshire.
With LARCs, "continuation rates are so much better than non-LARC methods," said Davis, who was not involved in writing the new AAP policy.
In her experience treating high school and college-age women, those who have used LARC methods have mostly been "quite happy" with the birth control, especially those women using IUDs, Davis said. "For the first time over the last couple of years, we have a large number of young women and adolescents coming and saying they want an IUD," she said.
Follow Live Science @livescience, Facebook & Google+. Original article on Live Science.
Is getting an IUD painful?
'Useless' female organ discovered over a century ago may actually support ovaries, study finds