Artificial Pancreas May Improve Type 1 Diabetes Treatment
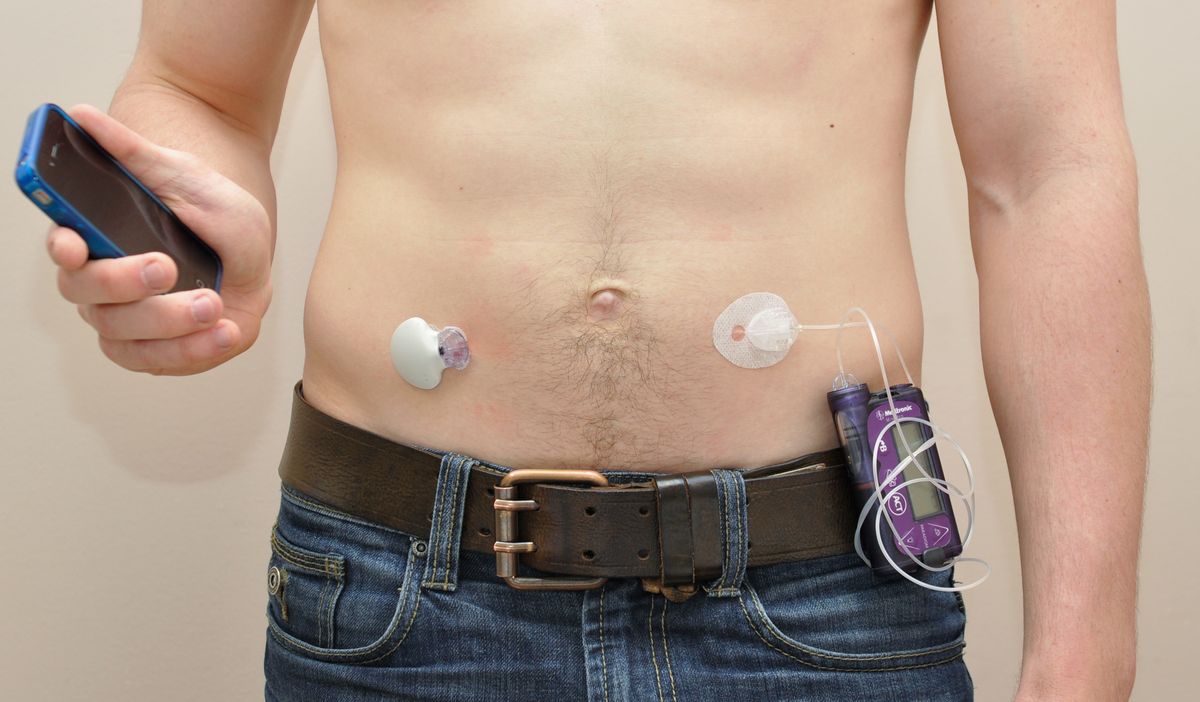
An artificial pancreas may offer people with type 1 diabetes a better way to their keep glucose levels in check than the conventional diabetes treatment, which involves an insulin pump, according to a new study.
The artificial pancreas is an automated system that helps people with diabetes control glucose levels through the automatic administration of one or two hormones.
In the new study of 30 adults and teens with type 1 diabetes, researchers compared the conventional insulin-pump therapy to two types of artificial pancreas. One type delivers two hormones, insulin and glucagon, while the other delivers only insulin. (Insulin triggers the cells in the body to take up glucose, so it lowers levels of sugar in the blood. Glucagon causes liver cells to release sugar into the blood, thereby raising blood sugar levels.)
The patients stayed overnight in a research facility three times between February 2013 and May 2014, and the doctors monitored the participants' glucose levels.
The researchers found that the patients' glucose levels were within the desired range 62 percent of the time during visits when the single-hormone artificial pancreas was used and 63 percent of the time when the dual-hormone artificial pancreas was used. In comparison, patients' blood sugar levels were within the desired range 51 percent of the time during visits when the insulin-pump treatment was used. [Bionic Humans: Top 10 Technologies]
"I think what we can say is that the artificial pancreas is definitely better than the conventional insulin pump," Dr. Betul Hatipoglu, an endocrinologist at Cleveland Clinic who was not involved in the study, told Live Science. "There is no question about it."
Moreover, the investigators found that, when either type of artificial pancreas was used, the patients experienced fewer incidents of the dangerous condition of hypoglycemia, compared with when the insulin pump treatment was used. In hypoglycemia, blood sugar levels drop too low, which can cause confusion and dizziness and, in severe cases, a loss of consciousness and coma.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
The researchers observed 13 cases of hypoglycemia, including five that were severe enough to cause symptoms, when patients were using the single-hormone artificial pancreas, and nine cases (none of which were symptomatic) that occurred when the double-hormone artificial pancreas was used. There were 52 such cases (12 of which were symptomatic) that occurred during the conventional treatment.
"Our study confirms that both artificial pancreas systems improve glucose control and reduce the risk of hypoglycemia compared to conventional pump therapy," study author Ahmad Haidar, of Institut de Recherches Cliniques de Montreal, said in a statement.
The researchers did not find any significant benefits to administering both insulin and glucagon, which is an emerging concept in the treatment of type 1 diabetes, Hatipoglu said. However, this study was small, and more research needs to be done to determine whether a single-hormone or double-hormone infusion should be used in an artificial pancreas.
The investigators also found that, with the use of either of the two types of artificial pancreas, no cases of hypoglycemia occurred at night while participants were sleeping, compared with 13 cases that were observed during the insulin-pump treatment, according to the study. None of those events were symptomatic.
"Given that low blood glucose remains very frequent during the night, the fear of severe nocturnal hypoglycemia is a major source of stress and anxiety, especially for parents with young diabetic children," study co-author Dr. Laurent Legault, a pediatric endocrinologist at the Montreal Children's Hospital, said in a statement.
The artificial pancreas is needed "immediately" in clinical practice, Hatipoglu said.
"These artificial pancreases are advancing very fast, and I hope we will have something in the market before 2020," Hatipoglu said. "This will improve the patient care dramatically, compared to [treatment using] the conventional insulin pump."
The new study was published today (Nov. 26) in the journal The Lancet Diabetes & Endocrinology.
Follow Agata Blaszczak-Boxe on Twitter. Follow Live Science @livescience, Facebook & Google+. Originally published on Live Science.