
Can Medical Marijuana Curb the Heroin Epidemic?

This article was originally published on The Conversation. The publication contributed this article to Live Science's Expert Voices: Op-Ed & Insights.
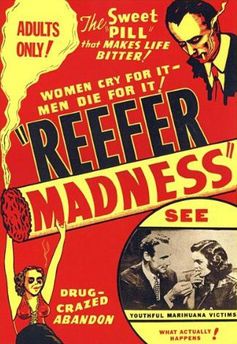
In the 1930s, Harry J. Anslinger, the first head of the Federal Bureau of Narcotics, embarked on a fierce anti-marijuana campaign. Highlighted by the 1936 anti-marijuana film Reefer Madness – where marijuana is depicted as a dangerous narcotic that makes good kids become sex-crazed killers – his propaganda efforts also maliciously linked marijuana use to African Americans and ethnic minorities.
By 1970, legislation codified cannabis as one of the nation’s most dangerous drugs: the Controlled Substance Act classified marijuana as a Schedule 1 drug, meaning it possessed high potential for abuse and had no acceptable medical use. Over 40 years later, the classification remains.
But research has shown that marijuana, while still criminalized at the federal level, can be effective as a substitute for treating opioid addicts and preventing overdoses. Massachusetts, which recently legalized medical marijuana – and where heroin overdoses have soared – could be a fertile testing ground for this potentially controversial treatment.
The medical case for marijuana
Before being criminalized, marijuana was used in the US to cure depression and a variety of other mental health ailments. Many studies have supported the therapeutic benefits of cannabinoids, along with the ability of marijuana’s psychoactive ingredients to treat nausea, help with weight loss, alleviate chronic pain, and mitigate symptoms of neurological diseases.
Other research, however, contradicts claims regarding the benefits of cannabidiol treatment. Some say marijuana actually poses a risk for psychosis and schizophrenia. Although the FDA has approved some synthetic cannabinoids for medical treatment, federal agencies do not support marijuana as a legitimate medicine until more clinical studies have been conducted.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
The scientific debate over the harms and benefits of marijuana has impeded federal lawmakers from moving forward on marijuana legislation reform. As a result, in 23 states, medical marijuana has become legalized by popular vote.
Marijuana policy dilemma
With each state crafting unique medical marijuana regulations, we find ourselves at a crucial turning point in drug policy. Public health professionals claim the road map used by “big tobacco” will be copied with legal marijuana, and addiction rates for marijuana will increase to those we see for tobacco. Others warn that if medical marijuana is used indiscriminately and without focused education on the uses and forms of medical marijuana, a prescription pain pill-like crisis could occur.
Among drug treatment specialists, marijuana remains controversial. Although some research has shown marijuana to be an alternative treatment for more serious drug addiction, addiction treatment specialists still view marijuana as highly addictive and dangerous. These views handicap policy reform, but despite its status as a Schedule 1 drug, recent research shows marijuana could be part of the solution to the most deadly drug epidemic our country has seen in decades.
Massachusetts: a case study
In 2012 Massachusetts became the 18th state to legalize medical marijuana, though the first 11 dispensaries are not scheduled to open until sometime in the coming year. This situation presents an opportunity to implement sensible, research-based policy.
Massachusetts, like many states across the US, has seen a dramatic rise in opioid addition fueled by the increase in opiate prescription pills. In Boston, heroin overdoses increased by 80% between 2010 and 2012, and four out of five users were addicted to pain pills before turning to heroin.
Meanwhile, the leading cause of death among the Boston’s homeless population has shifted from AIDS complications to drug overdoses, with opiates involved in 81% of overdose deaths. This is an alarming finding given recent expansion in clinical services for the city’s homeless.
Addiction specialists and health care professionals in Boston have been at the forefront of integrating behavioral and medical care. Naloxone and methadone are currently the main solutions to address the growing opiate addiction and overdose problem. But Naloxone is an overdose antidote, not a cure or a form of preventative therapy.
Methadone, like heroin and other opioids, has a very narrow therapeutic index (the ratio between the toxic dose and the therapeutic dose of a drug). This means that a small change in dosage can be lethal to the user. Marijuana, however, has one of the safest (widest) therapeutic ratios of all drugs.
Research shows that marijuana has been used as a form of self-treatment, where users take cannabis in lieu of alcohol, prescription opiates, and illegal drugs. That’s one reason why researchers are calling for marijuana to be tested as a substitute for other drugs. In this capacity, marijuana can be thought of as a form of harm reduction. While researchers don’t seek to discount some of the drug’s potential negative effects, they view it as a less damaging alternative to other, harder drugs. Despite these findings, marijuana is rarely incorporated in formal drug treatment plans.
A recent study might change this policy. Comparing states with and without legalized medical marijuana, it found a substantial decrease in opioid (heroin and prescription pill) overdose death rates in states that had enacted medical marijuana laws. In their conclusions, the researchers suggested that medical marijuana should be part of policy aimed to prevent opioid overdose.
Outside marijuana’s harms and benefits, missing in this discussion is the social environment of drug use. Drug use is social in nature. Where and with whom drugs are used influences why and how they are used. Socially acceptable or moderate use of drugs can be learned through social rituals in socially controlled settings.
Studies in the Netherlands found that using marijuana in Amsterdam coffeehouses encouraged a “stepping-off” hard drug use. These studies also found that when young people used marijuana in a controlled coffeehouse setting instead of a polydrug-using environment, they learned to use marijuana moderately without combining with other drugs. Along with providing access to marijuana, it’s important to instruct users on safe and effective medical marijuana consumption.
Since Massachusetts has not yet opened its medical marijuana dispensaries, it is too early to see if medical marijuana legislation will help reduce opiate addiction in the Commonwealth. Using recent research findings, Massachusetts policymakers have a unique opportunity to implement medical marijuana policies that address its contemporary opiate overdose. Medical marijuana could be part of drug treatment for heroin and opiates.
For homeless people, however, getting a marijuana card is expensive and buying medical marijuana from a dispensary is beyond their economic means. Street drugs are more prevalent in their social setting, easier to obtain, and can be much cheaper. From a policy perspective, addressing the alarming rates of overdose deaths among the homeless in Boston could mean distributing medical marijuana cards to homeless addicts for free and providing reduced cost medical marijuana.

Formerly demonized and later legislated as a Schedule 1 substance, marijuana could diminish the damage wrought by harder drugs, like heroin. While opioid use is a nationwide epidemic, Massachusettes – long at the forefront of developing scientifically based public policy – has the opportunity to be at the forefront of cutting-edge, socially-informed drug policy.
This is the second in a series of three articles on alternative strategies to treat addiction. To read the first in the series, click here.
This article was originally published on The Conversation. Read the original article. Follow all of the Expert Voices issues and debates — and become part of the discussion — on Facebook, Twitter and Google +. The views expressed are those of the author and do not necessarily reflect the views of the publisher. This version of the article was originally published on Live Science.












