Cough Medicine Ingredient May Aid Diabetes Fight

An ingredient in many over-the-counter cough suppressants seems to improve the release of insulin in humans, a discovery that may lead to new treatments for Type 2 diabetes.
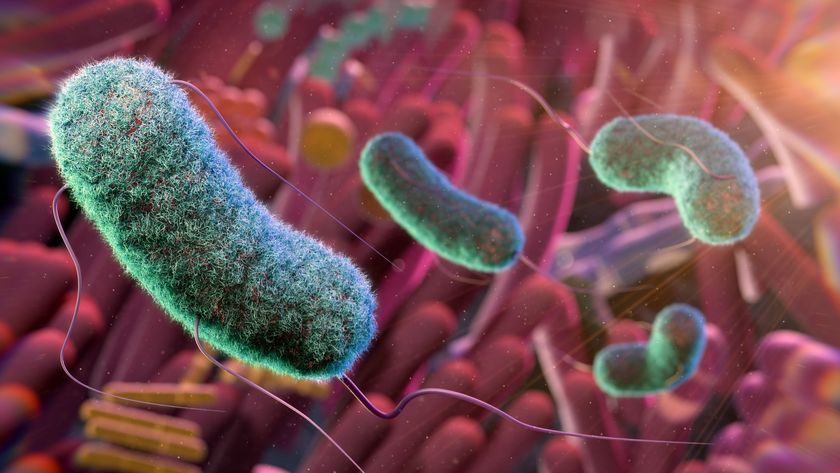
Doctors at Heinrich Heine University in Düsseldorf, Germany, found that the drug dextromethorphan increased the release of insulin from the pancreas in a series of studies conducted first in mice, then in human pancreatic tissue samples, and then in a small sample of people with diabetes.
Dextromethorphan, often indicated by the letters DM on the labels of cold medications, has few serious side effects, particularly in comparison to the current arsenal of drugs used to treat people with Type 2 diabetes, the researchers noted.
The results appear today (March 16) in the journal Nature Medicine.
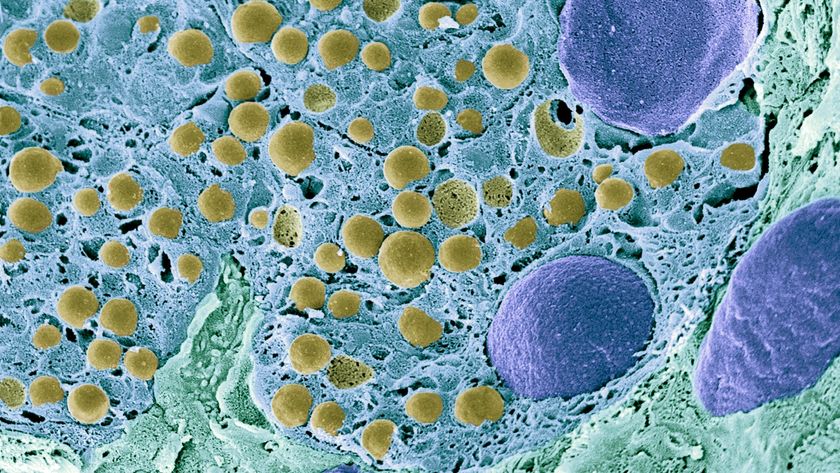
Type 2 diabetes affects about 350 million people globally, according to the World Health Organization. The disease is characterized by elevated levels of blood sugar, or glucose, which cells use for fuel. Insulin, a hormone produced in the pancreas, ferries glucose out of the blood and into the cells. But in people with Type 2 diabetes, the pancreas either does not produce enough insulin, or cells no longer respond properly to the hormone.
The authors of the new study said they stumbled upon the effects of dextromethorphan on diabetes by mistake. Based on the work that other researchers did a decade ago, they thought that dextromethorphan would suppress insulin secretion in patients with a condition called hyperinsulinism, which involves having too much insulin in the blood stream, somewhat opposite of diabetes. [7 Bizarre Drug Side Effects]
Instead, they found that dextromethorphan — or, more specifically, a compound called dextrorphan, which is a byproduct that forms in the body when someone takes dextromethorphan — increased insulin release from the pancreas.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Dextromethorphan works to stifle a cough by suppressing the activity of certain receptors, called N-Methyl-D-Aspartate (NMDA) receptors, in the medulla oblongata, which is a part of the brainstem just above the spinal cord, said senior author Eckhard Lammert, a professor of animal physiology at the Heinrich Heine University. NMDA receptors also are found in the insulin-producing cells in the pancreas.
The new findings show that suppressing the NMDA receptors in the pancreas enhances glucose-stimulated insulin secretion. Lammert said the finding surprised him, and it's not clear why it works that way.
The researchers warn that people with diabetes shouldn't begin to self-medicate with a dextromethorphan-based medicine. The human study, while promising in increasing serum insulin concentrations and lowering blood glucose, included only 20 participants.
"To date, we only have results from a single-dose clinical trial, which make us optimistic; but [this is] not sufficient to evaluate the clinical benefit of this drug for the long-term treatment of people with diabetes," Lammert told Live Science.
"My hope is that our study triggers further clinical trials at established diabetes centers," and that long-term clinical trials are also conducted, he said.
If it turns out that dextromethorphan does not work to control diabetes, then researchers could test other drugs that inhibit NMDA-receptors, to see their effect on controlling diabetes, the researchers said.
One of the authors of the paper, Dr. Jan Marquard, also of Heinrich Heine University, said that he is working on a new clinical trial investigating the effects of taking dextromethorphan along with the diabetes drug sitagliptin.
Follow Christopher Wanjek @wanjek for daily tweets on health and science with a humorous edge. Wanjek is the author of "Food at Work" and "Bad Medicine." His column, Bad Medicine, appears regularly on Live Science.

Christopher Wanjek is a Live Science contributor and a health and science writer. He is the author of three science books: Spacefarers (2020), Food at Work (2005) and Bad Medicine (2003). His "Food at Work" book and project, concerning workers' health, safety and productivity, was commissioned by the U.N.'s International Labor Organization. For Live Science, Christopher covers public health, nutrition and biology, and he has written extensively for The Washington Post and Sky & Telescope among others, as well as for the NASA Goddard Space Flight Center, where he was a senior writer. Christopher holds a Master of Health degree from Harvard School of Public Health and a degree in journalism from Temple University.