Not Just a Band-Aid: How ‘Smart Bandages’ Will Change Medicine (Video)
Charlie Heck, multimedia news editor at the U.S. National Science Foundation (NSF), contributed this article to Live Science's Expert Voices: Op-Ed & Insights.
Some bandages are embedded with medicine to treat wounds, but researchers have something much more sophisticated in mind for the future of chronic wound care — "smart bandages."
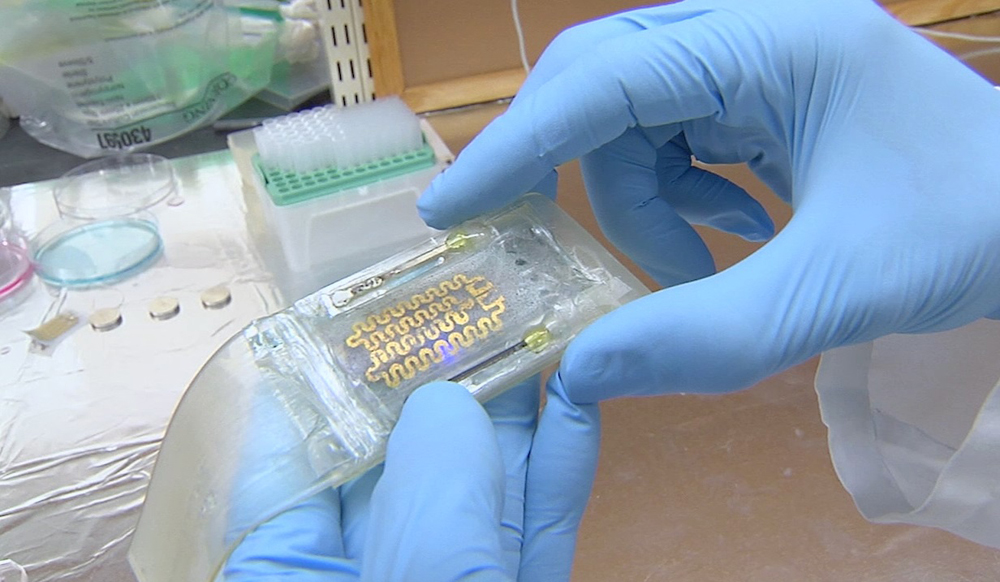
With support from NSF, a team of researchers from Harvard, Purdue, Tufts and Brigham and Women's Hospital is bringing together advances in sensors, biomaterials, tissue engineering, microsystems technology and microelectronics to create smart bandages for wounds that require ongoing care, such as burns, diabetic ulcers and bed sores.
The new devices, known collectively as flexible bioelectronics, will do much more than deliver medicine. They will be able to monitor all the vital signs of the healing process, such as oxygen levels and temperature, and make adjustments when needed, as well as communicate the information to health professionals who are off-site.
To fulfill the critical need for the devices to be flexible, the team is testing new materials, such as a hydrogel that would cover a wound with just the right amount of stretch to be comfortable.
Reza Abdi, associate professor in medicine at Harvard, is part of this research team. Below, Abdi answers questions about the research.
NSF: What are flexible bioelectronics?
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Reza Abdi: Flexible electronics is an emerging field which encompasses design and fabrication of electronic devices and circuits on flexible polymeric substrates. Flexible bioelectronics is the application of flexible electronics into biomedical and life sciences applications for monitoring, sensing and neuroprosthetics.
NSF: What are the types of particles you are making? How do they work with flexible bioelectronics?
R.A.: We are making polymeric and responsive microparticles (tiny, hollow particles) and embedding drugs inside them during the fabrication process. These microparticles can then release the drug when needed. The entire sensing and drug delivery system is made on a polymeric flexible substrate, hence flexible bioelectronics.
NSF: Can you take us through what exactly is going into these smart bandages and how the drug dispersal process works?

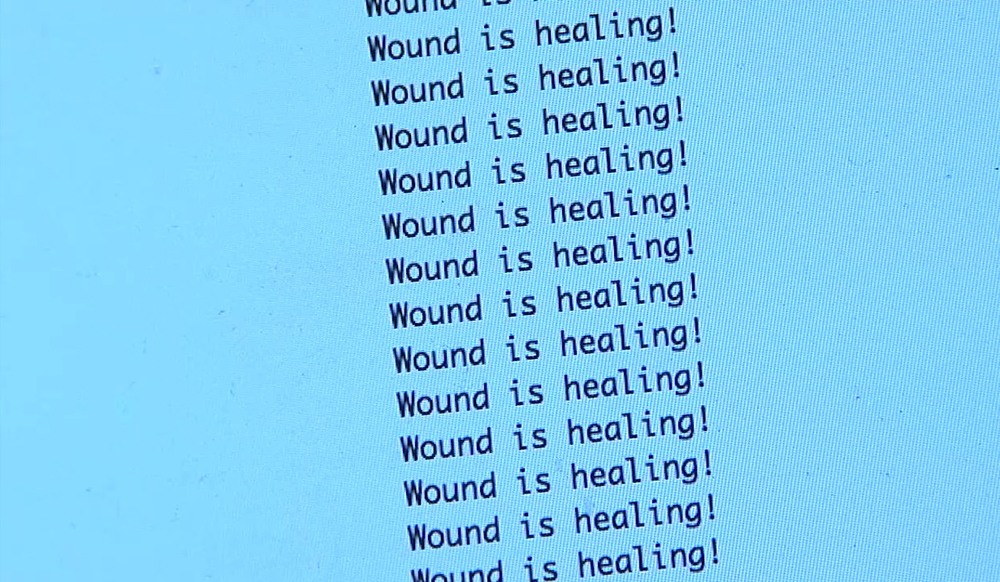
R.A.: We first create microparticles containing drug molecules and then incorporate these into a hydrogel patch that holds them. Next, we place a stimulation mechanism on top of the hydrogel patch. We monitor the wound area, such as its temperature and pH levels using flexible sensors. If the wound environment is outside normal conditions, then we send a pulse to the electrical stimulator which induces drug release from the microparticles.
NSF: What are some of the real world implications for this type of technology? And when could we start seeing these smart bandages being used?
R.A.: The goal is to have a smart band-aid system using flexible sensors and electronics. Current wound care or band-aid technology is designed to protect the wound area from environmental assault. However, it is a simple technology, which does not provide any information about the state of the wound. Our goal is to embed sensors and electronics to band-aids which will enable (i) real time monitoring of the wound environment and in case of a need, and (ii) intervene to remedy the external conditions (infection, etc.) by delivering drugs. We anticipate that such bandaids may be used on patients within five to ten years.
Follow all of the Expert Voices issues and debates — and become part of the discussion — on Facebook, Twitter and Google+. The views expressed are those of the author and do not necessarily reflect the views of the publisher. This version of the article was originally published on Live Science.
What are mRNA vaccines, and how do they work?
Deadly motor-neuron disease treated in the womb in world 1st