Innovative Wound-Healing Technique Could Save Limbs
The fight is on to save human limbs: As the rate of diabetes continues to rise, the foot ulcers and chronic wounds that can come with the condition — and can lead to amputations in severe cases — remain a persistent problem.
To address it, medical professionals are now turning to wound dressings made from human amniotic membrane, a tissue found in the human placenta.
With this innovative approach to treating wounds, doctors are giving another option to patients whose wounds won't heal using existing treatments. The method uses a substance that would otherwise end up discarded as medical waste following a birth.
"When you put membrane on the wound, the wound starts to heal faster," said Dr. Dusko Ilic, a physician and stem cell science professor at King's College London who specializes in regenerative medicine. In a new article, published Jan. 12 in the British Medical Bulletin journal, Ilic and his colleagues reviewed the use of medical products made from human amniotic membrane tissue to treat chronic wounds.
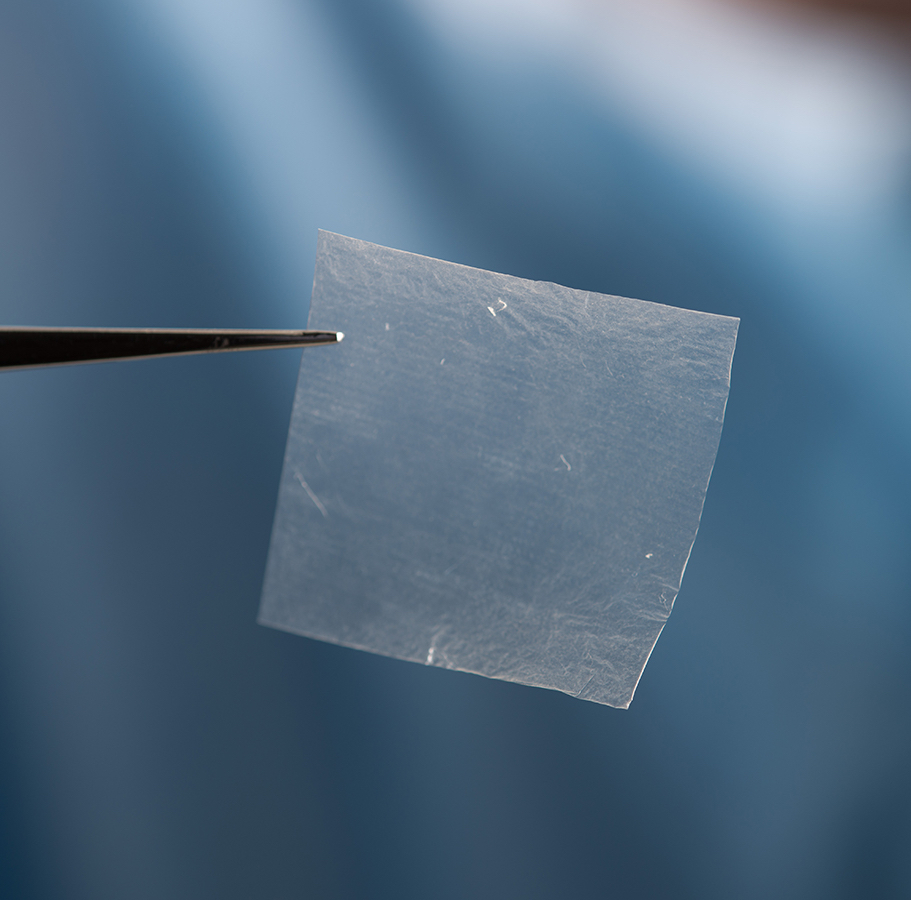
The human amniotic membrane is a thin, intricate protein mesh that covers the placenta as a fetus develops. When a pregnant woman's "water breaks," this is the protective layer that ruptures. Following birth, the membrane comes out of the woman's body along with the rest of the placenta.
The membrane resembles a piece of standard cling wrap, but it is full of growth factors, stem cells and nutrition for embryo development. The cells are stripped away when the membrane is prepared for use as a wound covering, leaving behind the protein scaffold, which is rich in one protein called collagen. [5 Amazing Technologies That Are Revolutionizing Biotech]
"What actually helps the healing is that intricate network of the proteins," Ilic said.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
When wounds don't heal
Diabetic ulcers affect 15 percent of people with diabetes during their lifetimes, and these wounds lead to more than 70,000 amputations annually, according to the Centers for Disease Control and Prevention.
The wounds develop because persistently high levels of blood sugar can damage nerves over time. This nerve damage, called neuropathy, interferes with the body's normal protective mechanisms. People with diabetes may not sense that they're putting too much pressure on one part of a foot for long periods of time, producing painful sores. The disease can also dry out skin, leading to cuts on the foot a person with diabetes may not even feel. Poor blood circulation means broken skin takes longer to heal, increasing the risk of infection.
Although studies have shown that wounds heal significantly faster when amniotic membrane products are used, Ilic found that there are only two major companies in Europe that are making products that use the membrane. The number of manufacturers is larger in the United States, but dressings made from the membrane still aren't commonly found in hospitals or clinics here.
"The wound-care community is relatively small," said Chris Liscio, director of regenerative tissue products at Derma Sciences, a medium-sized company in Princeton, New Jersey, that makes amniotic membrane dressings. Most diabetic wounds are treated by primary care physicians, or sometimes emergency doctors, he added.

Once ulcers set in, they can be difficult to heal, he said. In people with such wounds, "circulation is bad, nerves are damaged and sometimes [the wounds] persist for ages — for years," Ilic said.
The ulcers can lead to worse outcomes for patients. In one 2007 study, published in the International Wound Journal, researchers at Rosalind Franklin University in Chicago found that approximately half the patients receiving a diabetes-related amputation would not be alive in five years. That mortality rate is similar or worse than those of many common types of cancer.
For the toughest wounds, amniotic membrane really does help, Ilic said, especially those that haven't responded to other treatments. [Bionic Humans: Top 10 Technologies]
In one clinical trial, which tested a membrane product from Marietta, Georgia-based company MiMedx, researchers looked at 84 patients with diabetic ulcers ranging from 2 and 20 centimeters (0.79 to 7.9 inches) across. The ulcers had completely permeated the skin layers and still remained open after a month. The researchers treated the patients with either the membrane or traditional wound care, and then checked to see if the wounds were at least 40 percent closed within one month of treatment. Of those treated with an amniotic membrane product, 62 percent met the benchmark, compared to 32 percent who had received standard treatments, according to results published in 2014.
The idea of using this membrane is not new. In 1910, Dr. J.W. Davis at Johns Hopkins Hospital in Baltimore tried using the tissue as a skin graft and found it performed well. Throughout the early part of the century, medical researchers continued to experiment with the material, and found success using it for eye surgery.
Using the translucent membrane for wound dressings remained a fairly common practice until concerns about disease transmission interfered. The membrane was used less in the years after World War II, Ilic said. Then the rise of AIDS and other blood-borne diseases in the 1980s and 1990s caused the membrane to fall out of favor. Scientists turned to pigs and cows for skin substitutes.
However, within the past decade or so, researchers developed methods to safely test, sterilize and process the membrane for use in dressings, Ilic said. The membrane is used today most commonly as biological dressing in ophthalmology. Only within the past five years or so have specialists started using advanced amniotic membrane products to treat diabetic wounds.
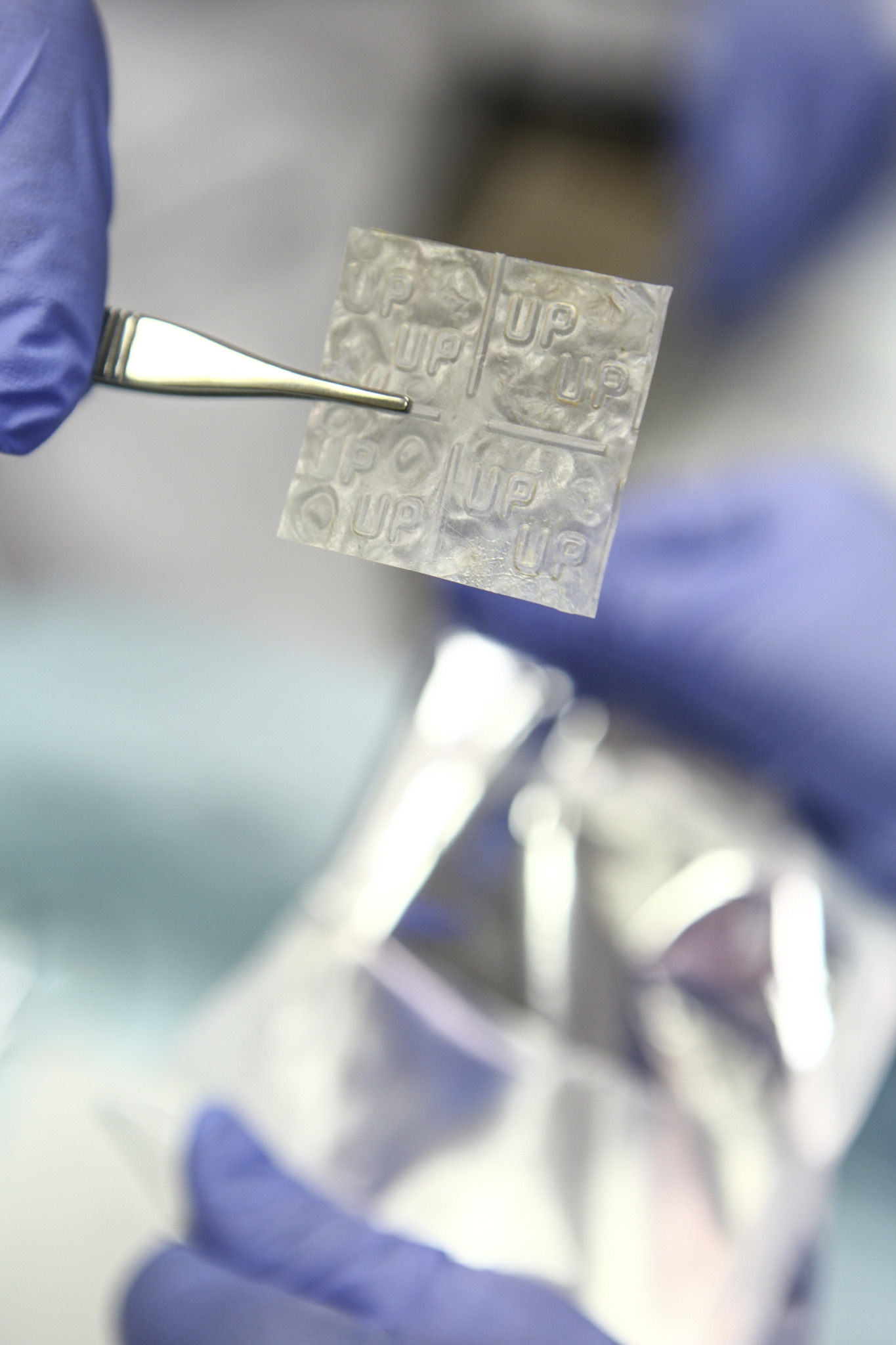
Several American companies make medical products from human amniotic membranes, including Derma Sciences, MiMedx and Osiris Therapeutics in Columbia, Maryland. Each company differs in how it processes the membrane, using proprietary methods. Liscio said there are generally two versions of the product, either cryogenically frozen or prepared for off-the-shelf use, like Derma Sciences' version.
Usually the companies collect membranes from women who have planned C-sections. That way, there is minimal damage to the placenta, Liscio said. Within hours of the membrane donation, the company begins processing the material.
MiMedx has a patented process called Purion for cleaning and preservation. Derma Sciences uses technology called Dryflex, which allows the final, sterile product to be stored up to five years.
Gaining wider use
While the products are available on the market and could potentially be employed by any physician, use currently tends to be limited to specialized wound care centers.
"Medical staff has to get it embedded in their heads," Ilic said. "This exists. This is really working."
Amniotic membrane derived from human tissue is relatively free of any significant side effects when used in the sheet form, said Dr. Donald Fetterolf, chief medical officer for MiMedx. Each membrane must be prepped and sterilized using strict American Association of Tissue Banks guidelines. "Tissue rejection or allergic reactions as a result have not been reported," he said. "The natural antigens that [would] identify a tissue as 'foreign' are not present in this unique environment."
The downside of using amniotic membrane products is that the cost to cover one wound can be incredibly high. "They're different sizes, but the price can range from $400 to $4,000 easily," Liscio said. Insurance coverage for amniotic tissue products varies widely as well.
The applications extend beyond aiding people with diabetes, to those with burns or diseases such as epidermolysis bullosa, a painful genetic disorder in which the skin surface peels away. For a patient with that condition, even using a towel would cause wounds, Ilic said. [Top 3 Techniques for Creating Organs in the Lab]
Additional randomized clinical trials are now underway for human amniotic membrane products, but these studies are expensive to conduct.
"Just like with every new medicine, it has to pass time and then people embrace it," Ilic said.
Liscio said he sees the field growing rapidly in the future. "The diabetes problem is not getting better," he said. "If you can do something to delay an amputation or even prevent it, the person could have a much better quality of life."
As for production, Ilic said he is confident plenty of amniotic membrane will be available. "Production is extremely cheap," he said. "And resources? The whole human race."
Follow us @livescience, Facebook & Google+. Original article on Live Science.









