
How Long Until Human Faces Can Be Printed in a Lab? (Op-Ed)

This article was originally published at The Conversation. The publication contributed the article to Live Science's Expert Voices: Op-Ed & Insights.
More than 30 people across the world have received face transplants since the first procedure was successfully carried out in France in 2005. The discussion has long since moved on from initial apprehensions to the practicalities involved in improving the technique. As a treatment for facial disfigurement which enhances quality of life, the clinical need is established and results to date have been encouraging.
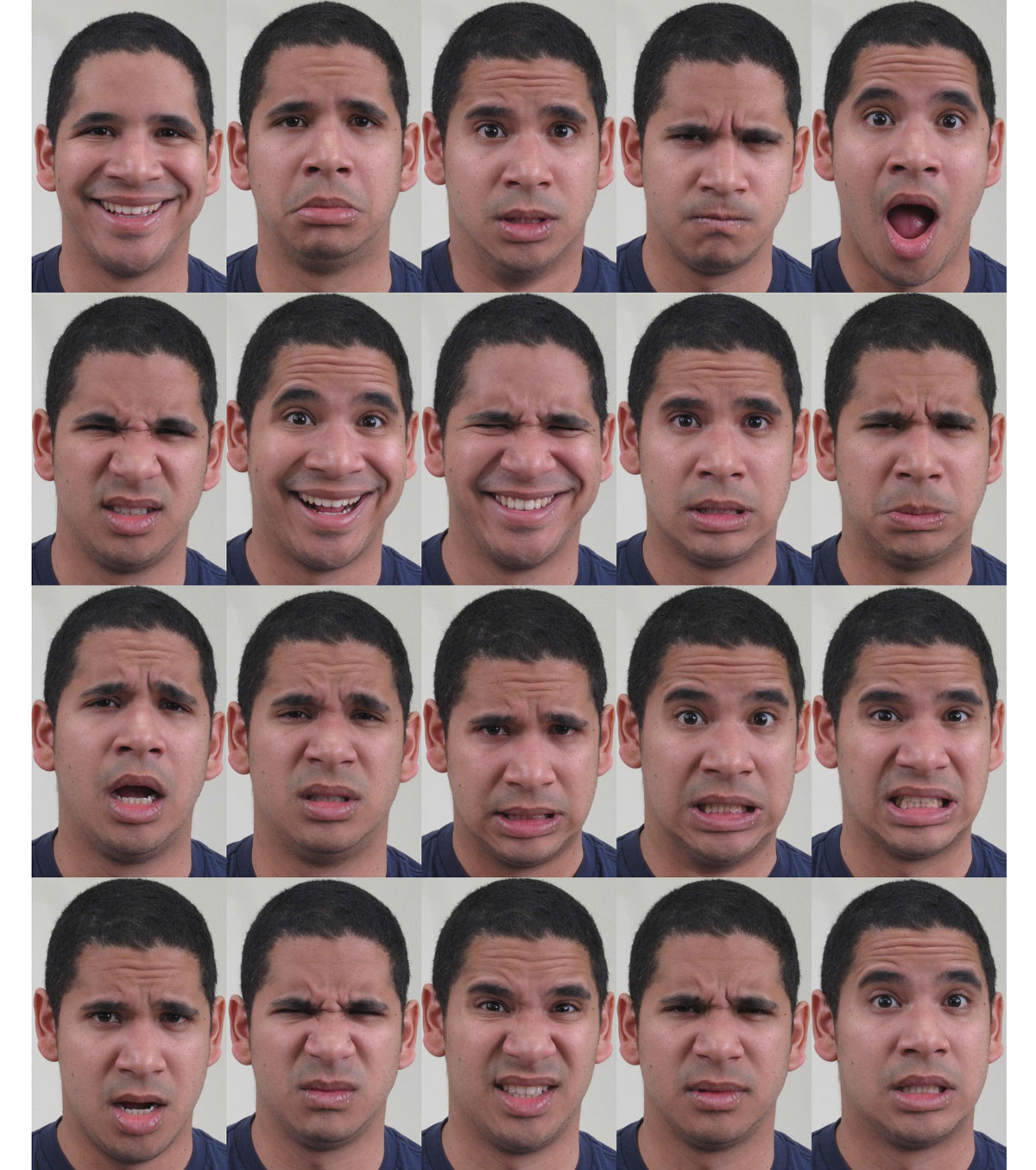
There is of course room for improvement, as the practice is still in its early days and rarely performed. Tissue rejection is a major issue for instance, meaning that the patient may need high doses of immunosuppressive drugs for life. Difficulties matching blood type, age, skin tone and hair colour are also preventing face transplants from becoming more routine.
These problems come down to the fact that the patient is receiving a face which previously belonged to somebody else. But what if a new face could be constructed from a patient"s own cells? Not a graft from elsewhere on the body, but a brand new piece of tissue which could be grown in the lab to the patient's specifications. How long until we can bypass face transplants and step into this other realm of possibility?
This is where stem cells enter the picture — specifically the variety that we call "pluripotent," which can renew themselves indefinitely and generate nearly every kind of cell in the body. Human pluripotent cells were first derived from donated surplus IVF embryos, but we can now create them by reprogramming mature cells such as those found in the skin. This means that you could take a skin biopsy, reprogram the cells into a pluripotent state, then use them as the starting point for producing many types of living tissue — including that of a person's face.
A layer of complexity
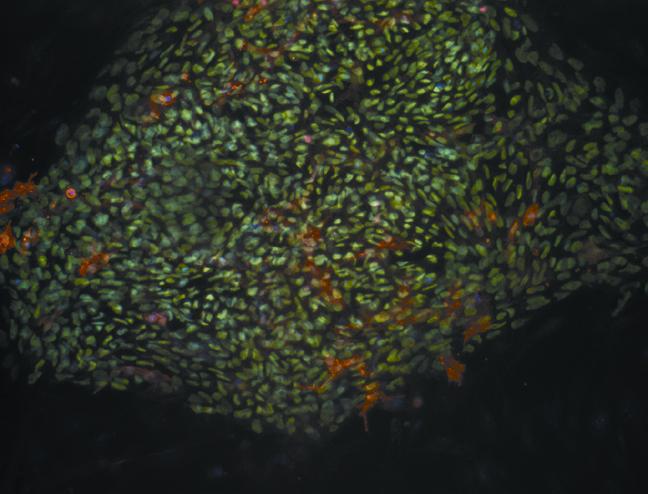
Creating skin is far more complicated than just producing one type of cell, but researchers across the field have already made some notable progress. Pluripotent cells have been used to produce many of the different cell types found in the skin, including the keratinocytes and melanocytes which are found in the outer layer (the epidermis), as well as the fibroblasts, adipocytes and macrophages which are found in the second layer (the dermis). In terms of generating complete tissue, US researchers have already combined fibroblasts and keratinocytes derived from stem cells to produce full-thickness artificial skin models. The inclusion of more cell types and complex functional elements such as hair follicles and sweat glands is a challenge for the future.
Much of the recent progress with cell production is the result of hands-on, small-scale laboratory work to produce tiny amounts of tissue. There is a long hop from here to producing sufficient numbers of cells to grow a face for transplantation. Yet technology is always advancing, and it is becoming easier to grow cells in larger numbers thanks to robotics and stirred-tank bioreactors. Techniques such as cell printing also now mean that complex tissue can be created by arranging cells into 3D structures. Such technology is again in its early stages, but could eventually be used for combining cells and structural proteins (sometimes referred to as bio-inks) to print an entire face from a template generated in software.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
While technical barriers are being eroded, the main shortcoming of using pluripotent cells to produce other cells at the moment is arguably function. Compared to the cells in the body, lab-produced cells often perform at low levels (for example, expressing fewer key proteins), though 3D tissue culture systems designed to mimic the environment in the body may go some way to addressing this.
Production techniques are also rarely fully standardised. Cells for transplantation need to be of the highest quality, and unless we can grow them to an adequate standard, transplantation could bring problems such as immune rejection or tumour formation.
Face value
If that all sounds like a long road ahead, the good news is that the journey will bring more immediate benefits in the fields of disease modelling and drug development. Human skin is already used to model conditions such as diabetic wound healing and skin cancer. As pluripotent cell technology matures, it will allow the large-scale generation of human tissue for examining a wide range of conditions, potentially providing better predictive capability than animal models.
In short, it is still hugely ambitious to think about deriving cells from a biopsy, generating and expanding a stem cell line, differentiating this into the various skin cell types, and engineering them into a piece of transplantable tissue. Even when we have solved the conundrums around cell function and scale of production, any technique for growing a face from one's own cells would require extensive safety testing. Recent progress with implanting retinal tissue derived from pluripotent cells into the eye of a Japanese woman is very encouraging, but we may still be looking at decades of development before we will be able to create skin for facial transplantation in a clinically workable timeframe. In terms of what could be achieved, we have barely scratched the surface.
Sebastian Greenhough, Research Technician, Glasgow Caledonian University










