Do People With Schizophrenia Really Have Multiple Personalities?
For people with schizophrenia, it can be difficult to determine what is real and what isn't. This chronic mental disorder is characterized by hallucinations and delusions — false beliefs, hearing voices and seeing things, among other abnormal perceptions — but do people with schizophrenia really have multiple personalities?
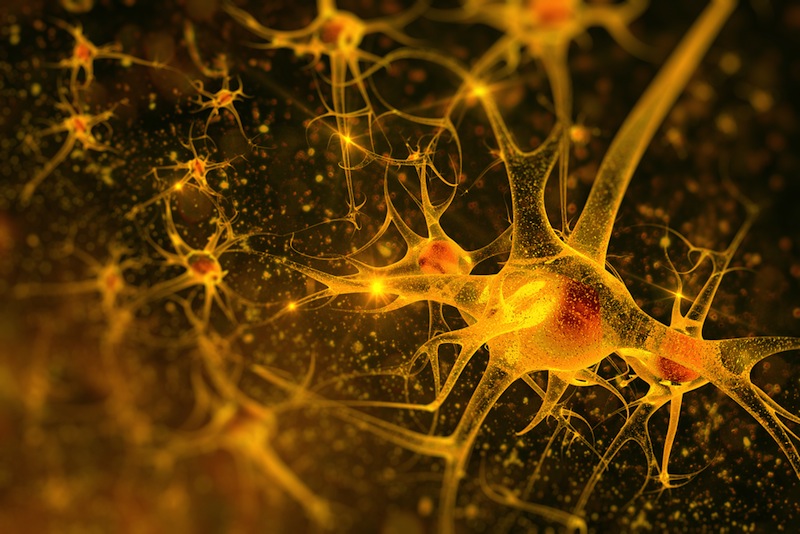
Schizophrenia actually refers to problems with hallucinations, not multiple personalities. In general, everything you see, hear, touch, smell and feel is processed by your brain. Special cells, called sensory receptors, take in information from the world around you and communicate the data to your mind, buthallucinations are sensory experiences without a stimulus — the brain is essentially getting faulty data. In people with schizophrenia, these hallucinations most commonly manifest as voices originating from inside the head or from a person who isn't there, according to the National Institute of Mental Health (NIMH).
Personality, on the other hand, is a different concept. The American Psychological Association defines personality as "individual differences in characteristic patterns of thinking, feeling and behaving." It can also be understood as "how the various parts of a person come together as a whole." [Top 10 Controversial Psychiatric Disorders]
Of course, if the information you're getting about where you are, what you're doing and who's around you is flawed, it could certainly have an impact on your cognition and behavior. But the idea that people with schizophrenia have more than one personality is a common misconception, experts said.
There is, however, an illness that causes people to adopt different personalities. That phenomenon is known as dissociative identity disorder (DID). Fluctuations in mood and behavior are normal for most individuals, but those with DID alternate among multiple identities, each with its own voice, characteristics and mannerisms.
DID is a "trauma-based illness," Dr. Randon Welton, an assistant professor of psychiatry at Pennsylvania State University's Milton S. Hershey Medical Center, said in a statement. According to the National Alliance on Mental Illness, DID is "more likely to occur in people who have experienced severe, ongoing trauma before the age of 5."
While the two disorders are different, they may have something in common. In the U.S., approximately 2.4 million adults, or 1.1 percent of the adult population, have schizophrenia, according to the NIMH. DID falls under the umbrella of general Dissociative Disorders, which, according to the the National Alliance on Mental Illness, affect an estimated 2 percent of the population. Experts have been long been interested in the biological origins of mental illness, and one idea in particular resurfaces about every generation: infection.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
With the advent of genetic research, "people thought there would be only 'brain genes' involved, but many [of the genes associated with these disorders] involve some aspect of the immune system," Dr. Robert Yolken, a virologist and infectious disease specialist at the Johns Hopkins Bloomberg School of Public Health in Baltimore, told Live Science. The idea here is that some sort of infectious agent (such as a virus) might trigger an immune response in the body that eventually leads to the development of a mental illness, he said.
"There's a subset of people with a degree of immune activation in the brain at the level of the glial cells," Yolken said. Glial cells are part of the nervous system but do not directly communicate via electrical signaling, or synapsing, the way nerve cells do. There are three types of glia: astrocytes, oligodendrocytes, and microglia, and they all function to support the signaling abilities of neurons according to the National Center for Biotechnology Information.
Glial cell inflammation could lead to hallucinations, rechanneling of the surfaces involved in memory and cognitive deficits — symptoms that can correspond with an illness like schizophrenia, Yolken said.
Some infectious diseases, like syphilis and malaria, are already known to induce psychiatric symptoms. But Yolken speculated that more common and even asymptomatic viruses, such as cytomegalovirus, which infects nearly one in three US children by age 5 according to the CDC, might trigger mental illness in individuals with a genetic predisposition. If an association is found between infections like CMV and mental illness, that could spur vaccine research or other public health measures, he said.
"Prevention is always better. In theory, if we could come up with infections that we know are more common, even though [psychiatric symptoms] only manifest in some people, it would be worth it" to develop vaccines against those infections, Yolken said.
Original article on Live Science.