Scientists Deliver Opioid-Like Pain Relief Without Addiction Risk

Scientists have created a drug that, in rhesus monkeys, can provide the same pain relief as opioid drugs, without the risk of addiction or other side effects.
Because a monkey's brain is so similar to the human brain, the drug is "highly expected to work in humans," said Mei-Chuan Ko, a professor of physiology and pharmacology at Wake Forest University School of Medicine, Winston-Salem, N.C., who led the study. He said that studies on humans could start in less than two years.
The research team said the new drug may one day provide relief for people with chronic pain while also quelling the rising abuse of opioids, which now account for the majority of drug-overdose deaths in the United States, according to the Centers for Disease Control and Prevention. Their work appears today (Aug. 29) in the journal Proceedings of the National Academy of Sciences. [5 Surprising Facts About Pain]
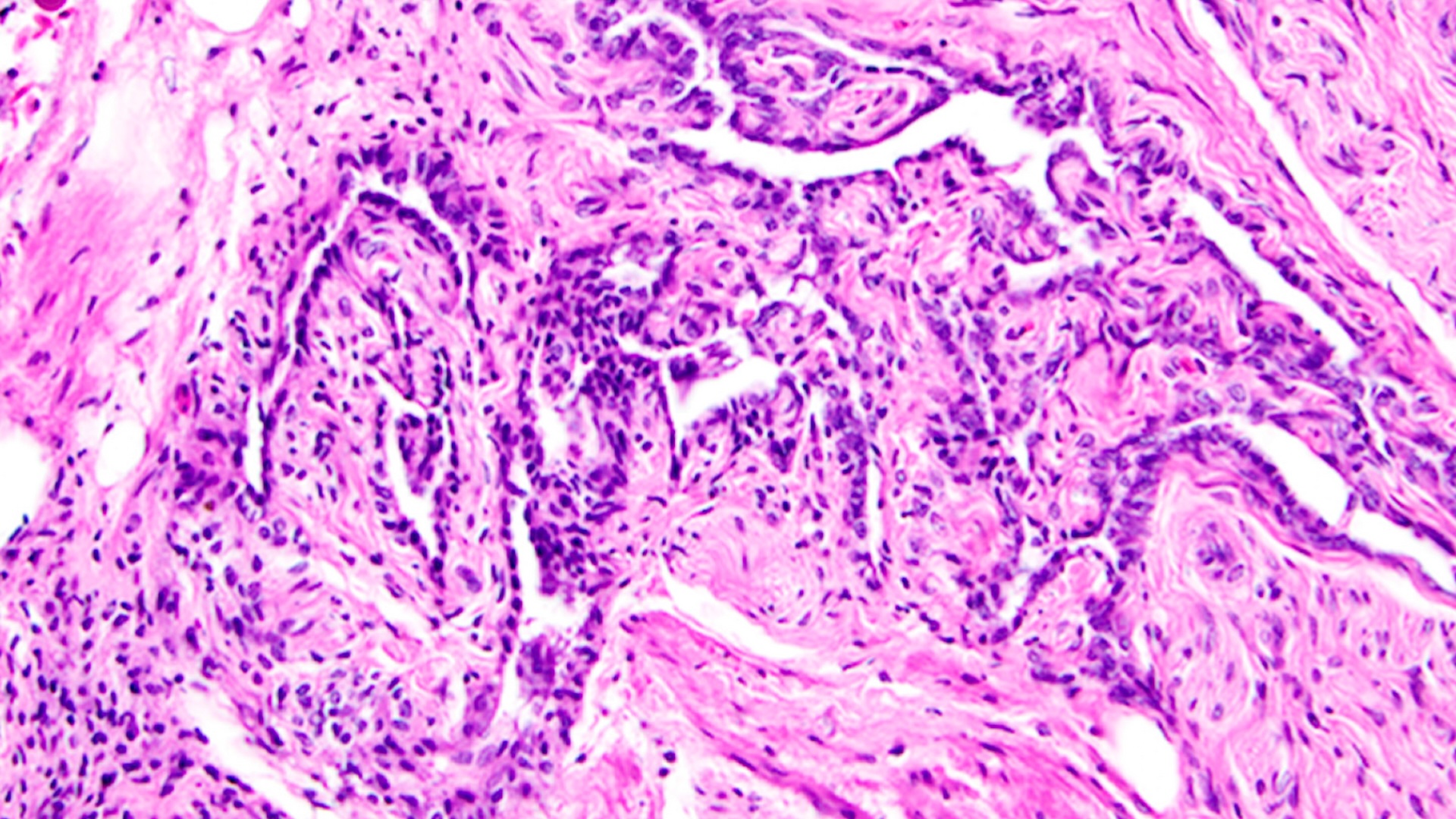
Opioids have been used for centuries to provide pain relief. They include heroin, morphine, codeine, and prescription drugs such as Vicodin and OxyContin. They work by reducing the intensity of pain signals reaching the brain, primarily by interfering with neuron cell receptors known as opioid receptors. A primary target for opioid drugs is a particular receptor called the mu opioid peptide receptor (MOP).
Opioids are highly addictive, however, because these same opioid receptors that respond to pain signals also involved in regulating emotional impulses such as the desire for reward, euphoria and cravings.
Previous research has found that drugs that target another neuron receptor called the nociceptin-orphanin FQ peptide receptor (NOP) can block the addictive effects of opioids. So, Ko and his colleagues took a dual approach by creating a drug analog that could simultaneously target both the MOP and NOP brain receptors to produce opioid-like pain relief while reducing the risk of addiction.
Stephen Husbands, a professor of medical chemistry at the University of Bath in England, created the dual-receptor-binding drug, called BU08028. Ko's group tested this in monkeys and indeed found that it produced pain relief with no signs of being addictive. The monkeys did not self-administer the drug as they typically would with opioids or other addictive substances such as cocaine, Ko told Live Science.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
The drug analog BU08028 also had no apparent side effects, Ko said. In contrast, opioids can cause respiratory failure and cardiac arrest, major causes of death from opioid use. Ko said that BU08028 did not cause such side effects in monkeys even at 10- to 30-times the dose needed to relieve pain .
The research team has high hopes that the BU08028 compound would be effective in humans.
"Non-human primates such as rhesus monkeys have similar physiological responses to opioid analgesics like humans," Ko told Live Science. "They serve a surrogate species for humans in the research and development of opioid-related compounds."
Ko added that the one obstacle in creating an effective drug for humans may be in optimizing the therapeutic effect of the drug when making it in a pill form. This would be a major focus of any clinical study.
Follow Christopher Wanjek @wanjek for daily tweets on health and science with a humorous edge. Wanjek is the author of "Food at Work" and "Bad Medicine." His column, Bad Medicine, appears regularly on Live Science.

Christopher Wanjek is a Live Science contributor and a health and science writer. He is the author of three science books: Spacefarers (2020), Food at Work (2005) and Bad Medicine (2003). His "Food at Work" book and project, concerning workers' health, safety and productivity, was commissioned by the U.N.'s International Labor Organization. For Live Science, Christopher covers public health, nutrition and biology, and he has written extensively for The Washington Post and Sky & Telescope among others, as well as for the NASA Goddard Space Flight Center, where he was a senior writer. Christopher holds a Master of Health degree from Harvard School of Public Health and a degree in journalism from Temple University.