How Do Antibiotic-Resistant Bacteria Get into the Environment?

This article was originally published at The Conversation. The publication contributed the article to Live Science's Expert Voices: Op-Ed & Insights.
Antibiotic resistance is a growing public health problem. The United Nations recently acknowledged this as "one of the biggest threats to modern medicine," dedicating a high-level meeting to the issue at the 2016 General Assembly.
In the U.S. at least 2 million people are infected with antibiotic resistant bacteria and 23,000 die each year. This problem is largely due to misuse of antibiotics.
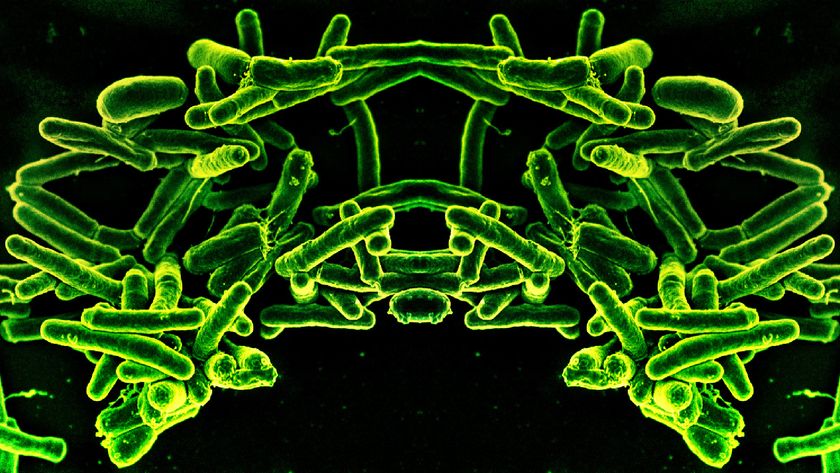
Research on antibiotic resistance tends to focus on infection control in hospitals and development of new drugs. But antibiotic bacteria aren’t just found in hospitals or clinics. They – and the genes that confer resistance – are found in the environment, too.
People carry all kinds of bacteria, potentially even resistant bacteria, in and on their bodies. People can shed these bacteria in communal spaces such as locker rooms or even beaches, but a major concern is their presence in human sewage. Resistant bacteria enter our aging sewer infrastructure and may eventually end up in the environment through sewage spills. This can expose people to hard-to-treat infections, and creates the potential for genes conferring resistance to be spread to other bacteria in environmental habitats.
At the Harwood Lab at the University of South Florida, we study how resistant bacteria survive in the environment and the impact sewage entering recreational waters might have on human health. In fact, we found vancomycin resistant enterococci (VRE), one of the most common causes of hospital acquired infections, in water and sediment near St. Petersburg, Florida after a domestic sewer line break in September 2014.
Sampling water and sediment near a sewer line break
In Florida, hurricanes and tropical storms mean that sewage discharges, septic system failures and sewer line breaks happen frequently during the rainy season.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
That’s what happened in Pinellas Park, Florida in September 2014. A sewage pipe broke near a school, forcing cars to detour around a parking lot flooded with thousands of gallons of raw sewage. One of the causes was probably was the 3.3 inches of rain fell in the area the weekend before the pipe broke.
We sampled water and sediment from the site of the initial line break for seven weeks following the spill event, testing samples for enterococci, fecal bacteria used as water quality indicators and surrogates for pathogens. We then used similar methods to test for VRE.
We also looked for the vanA gene, which can confer resistance to the antibiotic vancomycin. One of the most interesting, and worrying, facts about antibiotic resistance is that resistance genes, like vanA, are often mobile. These genes can be carried on mobile genetic “cassettes” called transposons. These transposons frequently contain multiple antibiotic resistance genes and can be shared from one bacterium to another (called horizontal gene transfer).
vanA genes are known to be carried on transposons that can be easily transferred, which are strongly associated with the spread of VRE infections in hospitals.
Finding resistant bacteria and resistance genes in sewage
Vancomycin resistant enterococci have very rarely been detected in surface water or sewage in the U.S., so we weren’t expecting to find these bacteria in the water and sediment from the drainage ditch at the site of the spill. But we did, as well as thousands of garden-variety enterococci per liter of water. VRE grown in culture were detected up to three days after the date of the spill.
VRE are considered a serious health threat by the CDC, infecting 20,000 people and killing over 1,000 per year. As VRE become increasingly prevalent in hospital settings, it is inevitable that some individuals carry a remnant VRE population when they leave the hospital. These VRE are essentially part of the “normal flora” of these people, and can be passed to others. And people in good health can be colonized by these bacteria without any symptoms.
In this way, VRE can spread within the community. Although miles from any major hospital, the “community sewage” in this sewer line may have been collecting the waste of people recently treated with vancomycin or those colonized with VRE.
The vanA gene was detected in water and soil up to 12 days after the spill. It is likely that VRE and their resistance genes are found in sewage throughout Tampa Bay and the rest of the country.
Outside of the hospital, a major concern is that other harmful bacteria or even innocuous environmental microbes may acquire these genes when exposed to raw sewage that contains them. The more abundant these genes are in the environment, the more likely they are to be transferred to other, potentially harmful bacteria.
This doesn't just happen in Florida
This study examined one sewage spill in one city, but the repercussions are wide and the parallels to other communities are strong.
Consider New York City, where combined sewer overflows dump a mix of sewage and stormwater into the Hudson River almost every time it rains, or Rio de Janeiro, where Olympic athletes dosed themselves with antibiotics and home remedies in attempts to combat the high concentrations of resistant bacteria and viruses in the sewage-contaminated waters where they competed.
Other studies in this field have found resistance genes in animal agriculture waste and the feces of wildlife. However, another study suggests that almost all resistance genes are removed from sewage when fully treated by wastewater treatment plants.
But more surveillance of resistant bacteria and related genes is necessary. Not only do we need to understand what is going on after sewage line breaks, but we need to get a sense of what genes and resistance bacteria are living in environment the rest of the time.
Suzanne Young, Ph.D. student, University of South Florida and Valerie Harwood, Professor of Biology , University of South Florida
This article was originally published on The Conversation. Read the original article.
Most Popular