Thanks, Fido! Cancer Drugs Tested on Pets

Last December, Luisa Bozano's dog Einstein was diagnosed with brain cancer. The large tumor took up most of the 8-year-old boxer's left brain lobe. With few options, the owner settled on surgery to remove as much of the tumor as possible, along with half of Einstein's skull, which was replaced it with a polymer-based cement.
Things were going well until mid-year, when the tumor came back.
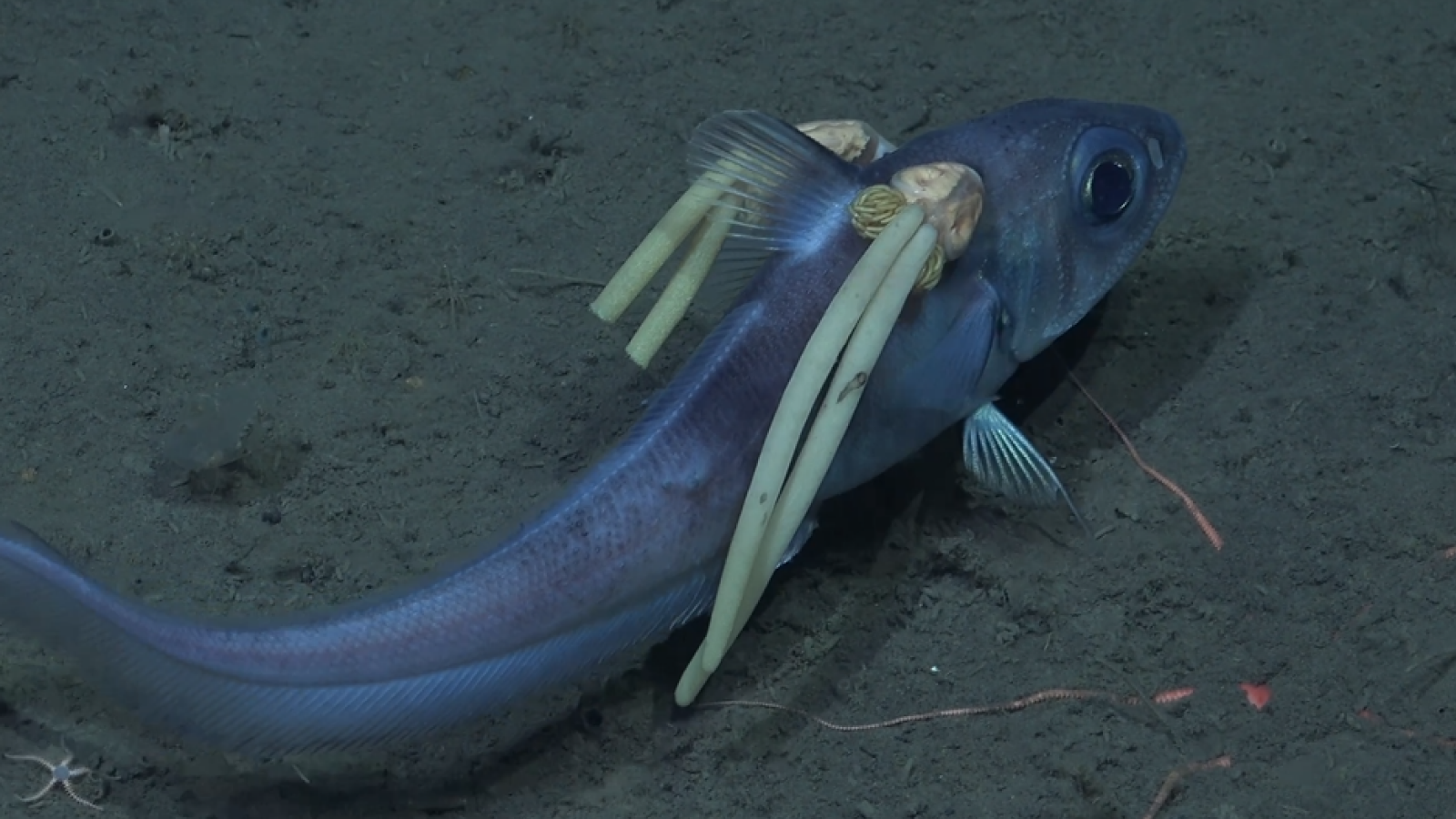
Now, it had tentacles, like an octopus weaving its arms through the vital organ's neural cells. The only treatment option left that might thwart the tumor's progress was an experimental therapy that involved injecting a virus into the dog’s brain. The virus would theoretically infect only the rapidly-dividing cancer cells, and later, an anti-viral treatment would be administered to kill the virus along with the infected tumor cells.
The scientists plan to someday use the therapy in humans. But Einstein would become the first being to test it out.
"He’s very bad, and this is his only shot," Bozano said.
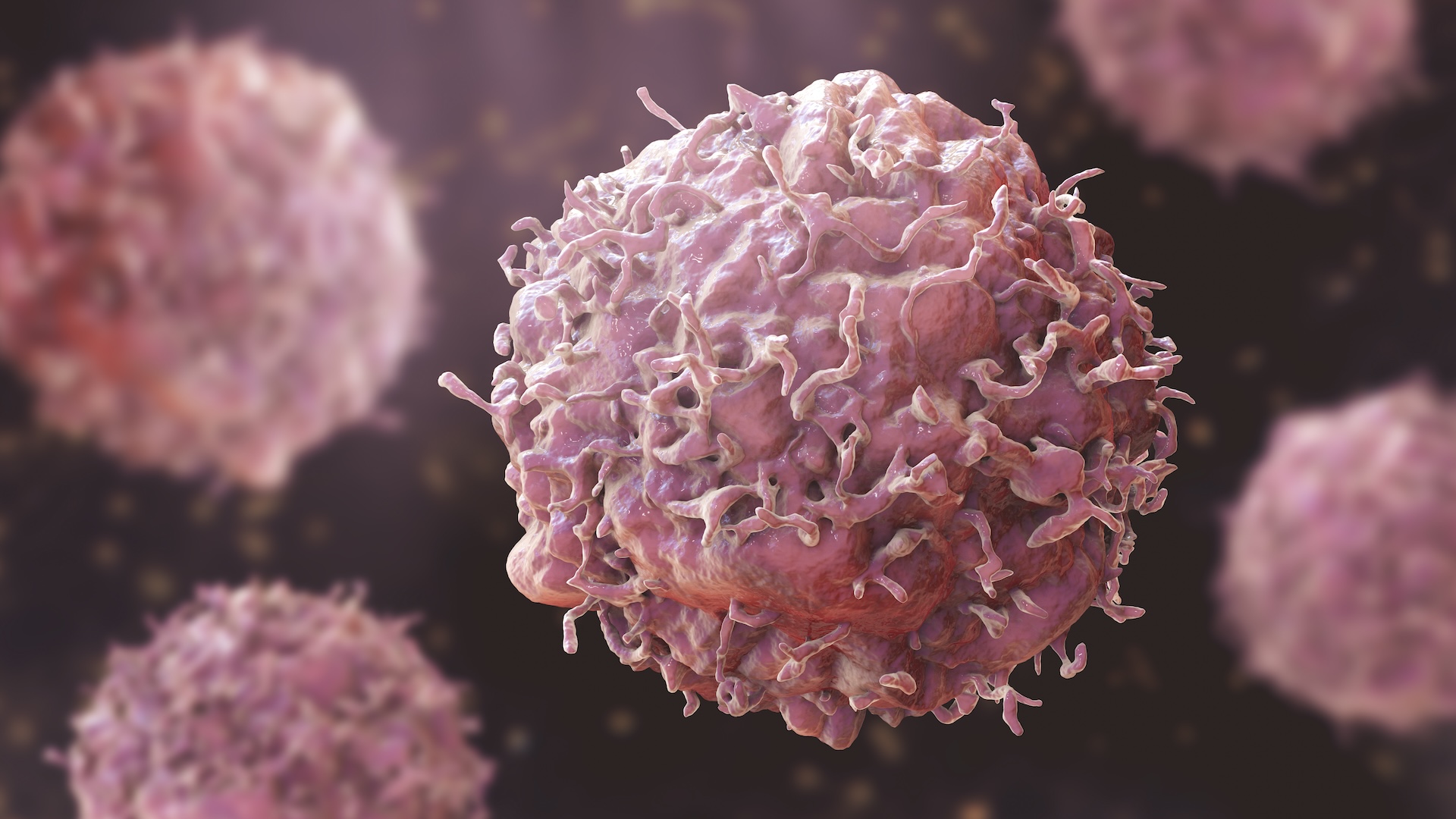
Einstein is one of about 6 million dogs diagnosed with cancer in the United States each year. From this large group, a new research field is growing, known as comparative oncology, which uses companion animals (mostly dogs) as models for human cancer. Cases like Einstein's provide a unique opportunity for scientists to test out novel cancer therapies on naturally arising tumors, as opposed to the artificial tumors typically induced in lab animals. Researchers hope the knowledge that stems from these therapies could help both people and their furry friends.
Recent strides
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
This isn't the first time dogs have been used as models for cancer research. They were guinea pigs for human bone marrow transplantation methods in the 1960s and 70s, and limb-sparing procedures for bone cancer in the 1980s and 90s.
But in recent years, scientists have realized that there is huge potential for pets to help us in the fight against cancer, and in 2003, the National Cancer Institute (NCI) founded the Comparative Oncology Program. This program aims to use pets to learn more about the biology of cancer and help test and refine novel therapies for translation to human cancer patients.
"For 20 or 30 years, we've been able to say, the comparative approach has made a valuable contribution to the field of science, and most particularly, the field of understanding and treating cancer," said Dr. Melissa Paoloni, a veterinary oncologist and NCI researcher. "However, in the last four or five years, the strides have been much more significant."
The complete sequencing of the canine genome in 2005 advanced the field even further, as scientists can now study the genetics of dog cancer and apply that knowledge to human cancers.
Why Fido?
Why use pets? For one, cancers in companion animals arise spontaneously, like cancers in humans.
"The disease of cancer in our pet animals is much more complex and sophisticated than what we can replicate in the laboratory," Paoloni said. "All of the problems with cancer that human patients have are mirrored in our pet population."
Like human cancers, pet cancers can become resistant to chemotherapy, can reoccur after treatment and can metastasize, or spread to other areas of the body, which can be "a terminal diagnosis for all cancer patients, regardless if they have fur or not," Paoloni said.
Another big advantage is that scientists can evaluate new treatments on pets fairly early on in the cancer's progression, whereas, with people, they might have to use the new therapy as a last resort when the cancer is significantly advanced.
“We may be essentially disadvantaging therapeutic strategies that might work in an upfront setting by choosing the worst population of [human] patients to test,” said Dr. Barbara Kitchell, director of the Center for Comparative Oncology at Michigan State University's College of Veterinary Medicine. But in pets, scientists can use experimental treatments right away since there are no set standards of care for animal cancers, and they are able to have a better understanding of what the outcome might be if the tumor is treated early.
Humans and their pets also usually share a similar environment. That means dogs are exposed to some of the same cancer-causing agents as their owners, and may develop similar cancers from these environmental factors.
Since dogs generally have a shorter lifespan than people, their cancers will progress more rapidly than human cancers, allowing scientists to see the disease outcome in a shorter timeframe. “If you had a treatment and you’re waiting to see the five- or 10-year survival follow-up be in a person, that timeline is really compressed in the dog,” Kitchell said.
A “different spectrum” of cancer
When dogs and people have the same type of cancer, the biology of the disease can be quite similar, Kitchell said. But the frequency of the different cancer types varies between the species. “[Dogs] have a different spectrum of disease,” she said. Some cancers that are common in people, such as breast and prostate cancer, are rarely seen in dogs because they are spayed and neutered. Also, dogs don’t get lung cancer as often, because they don’t smoke; and their high-fiber diets protect against colon cancer.
But cancer research in dogs can still inform cancer research in humans, even if the cancers are not the same. That's because two different cancers may be very similar at the molecular level — the cellular process that leads to skin cancer in dogs could resemble the process that leads to breast cancer in women, for example. Scientists can take advantage of this similarity to use dog models to develop a human therapy targeting that cellular pathway.
Additionally, some rare cancers, so-called “orphan diseases” in people, are not so rare in dogs. For example, dogs, especially large breeds, are much more likely than humans to get bone cancer, a disease that primarily affects children.
Scientists can take advantage of these high rates of rare cancers, and use dogs to study “orphan diseases” on a larger scale than they would perhaps be able to in humans. “It’s very hard to get enough human beings together to model [a rare cancer], but we can do that in the dog very easily,” Kitchell said.
Guiding drug development
Researchers and pharmaceutical companies have been able to use dog models to help them design human clinical trials and develop new cancer drugs. For example, from 2003 to 2006, Dr. Phil Bergman of the Memorial Sloan-Kettering Cancer Center in New York used dogs to develop a vaccine for melanoma, or skin caner. The vaccine was approved for use in dogs in 2007, but the research results have aided scientists that are working on a similar vaccine for humans.
"Data generated in trials in pet dogs can be used to help guide the design of human clinical trials," Paoloni said. These trials can help scientists learn how to use the new drugs at an optimal schedule, understand what drug levels to aim for, and examine adverse events or toxicities that might be associated with the therapies, she said.
Testing out new therapies in dogs and other pets does have a down side. Therapies might be so tailored to work in animals that they do not translate across species. Also, pharmaceutical companies worry that drugs that may be perfectly safe to use in people could have bad side effects in dogs, Kitchell said.
“What if they encounter a side effect in a dog trial that puts in jeopardy a lead compound that the company is testing for FDA approval, and now they have to explain why dogs have this toxicity, but people would never experience the same thing,” she said, referring to the Food and Drug Administration.
Even so, pharmaceutical companies welcome the opportunity to have new models that might aid them in the very costly and usually unsuccessful process of drug development. A new oncology drug costs about $1 billion to develop, and only about 5 percent of all oncology drugs ever make it to the market, Paoloni said.
"That amount of attrition and loss in the process, and the expense of that loss really has also made the drug development community more interested in finding new models," she said.
Personalized medicine
In the future, doctors hope to be able to tailor cancer therapies to an individual's tumors. Called "personalized medicine," such therapies involve taking a sample of a tumor, analyzing its genetics, and coming up with a prescription that is designed to treat that particular cancer.
But before the era of personalized medicine arrives, Paolini said comparative oncology is the best model for scientists to truly study this type of individualized therapeutics.
"I see the development of personalized medicine strategies as being one of the most unique and interesting contributions of the comparative approach that we're going to see come to fruition over the next few years," she said.
For dog owners such as Bozano, taking part in a clinical trial for a novel therapy offers a final chance to take action that may keep her dog alive. “That was to us the last hope, the last thing to try,” she said.
And in Paoloni's experience, owners want to enroll their pets in these clinical trials, not only to help other animals, but also to help people. "Knowing that studies used via the comparative approach will also be used to help human patients, I think that's been a very valuable teaching point and motivation for the client-owning pet community." Paoloni said

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.