Italian Island's Mutation Fights Malaria, But Raises Risk of Other Diseases
When it comes to human evolution and survival, fighting off one disease can sometimes mean that a person becomes more susceptible to another.
In the latest example of this finely balanced fight, new research reveals that a genetic mutation that increased resistance to malaria in one group of people also increased their rates of the autoimmune diseases of multiple sclerosis and lupus. Autoimmune diseases are conditions under which the immune system attacks the body's own tissues.
By identifying the gene mechanism at play, the researchers said they may have illuminated a way to tamp down the haywire autoimmune responses that lead to multiple sclerosis and lupus. [The 7 Biggest Mysteries of the Human Body]
"I am hopeful that the approach we employed in the work will be useful to identify new targets for therapy that will led to better treatments for these diseases," said FrancescoCucca, director of the National Research Council's Institute of Genetic and Biomedical Research in Italy, in an email to Live Science. Cucca is one of the senior authors of the study, which was published today (April 26) in the New England Journal of Medicine.
For the study, researcherscombed through genetic data from people living on Sardinia, an Italian island. Although people thereare famousfor their longevity, the population also has some of the world's highest rates of multiple sclerosis and lupus.
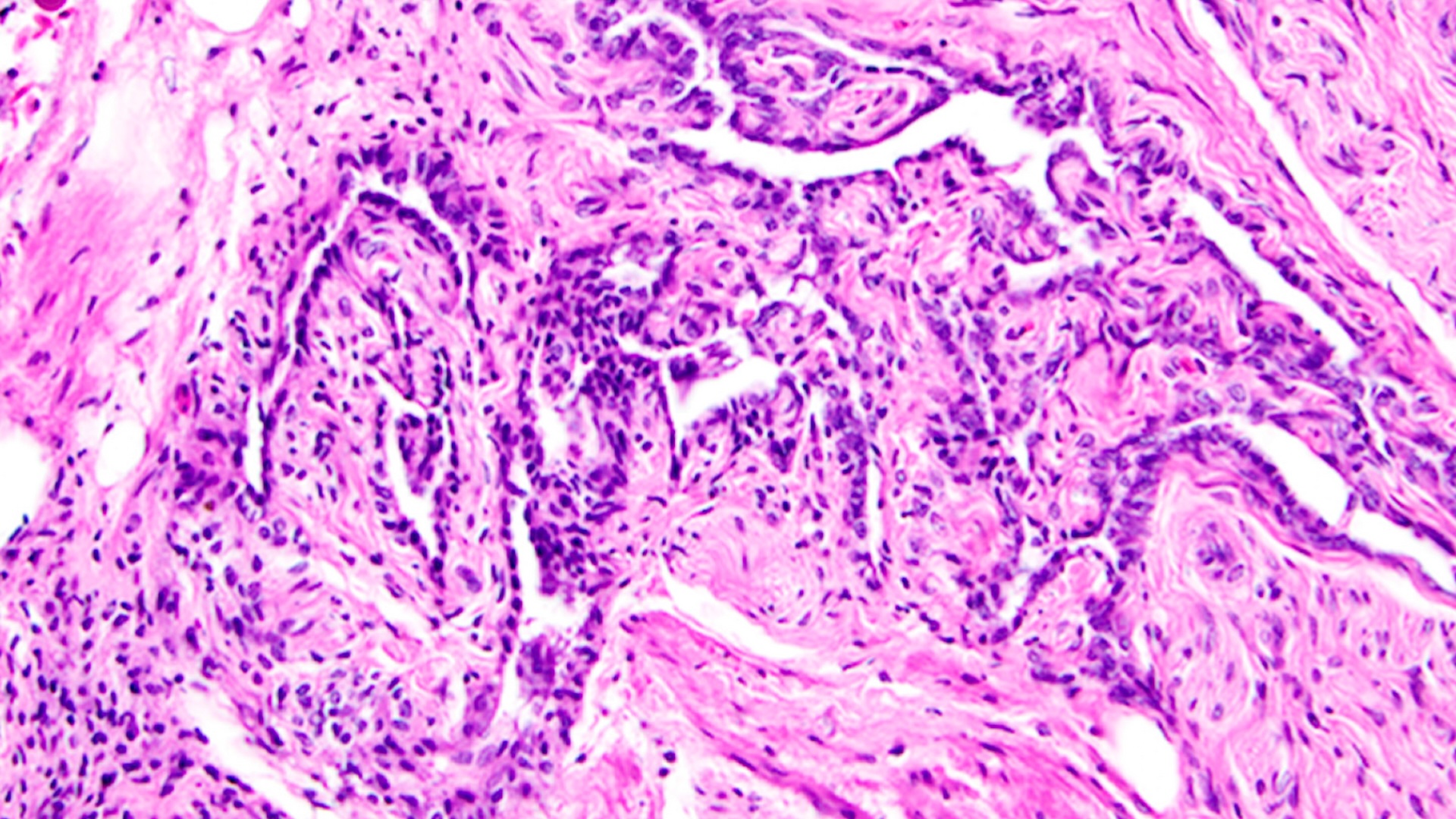
After analyzing more than 2,000 patients from Sardinia who had either multiple sclerosis or lupus, as well as a control group of more than 2,000 Sardinians without those diseases, the team zeroed in on a genetic mutation in a gene called TNFSF13B. This gene encodes a protein known as the B-cell activating factor — or BAFF — which, in turn, plays a role in unleashing the body's infection-fighting B cells.
Although B cells are effective at fending off infectious diseases, in people with multiple sclerosis, they're thought to lead the charge in the immune system's self-sabotaging attacks on the protective covering around nerve cells. In those people who have lupus, B cells also play a leading role in attacking the body's own healthy cells and tissues.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
The Sardinian patients with the TNFSF13B mutation showed unusually high levels of the BAFF protein, which caused high levels of active B cells. When the researchers compared the Sardinians' genomes with control groups of healthy people, and with people with lupus and multiple sclerosis from mainland Italy, Sweden, the UK and the Iberian Peninsula, they found that the form of the TNFSF13B mutation on Sardinia does exists elsewhere, but it's relatively less common.
The researchers speculated that the mutation's prevalence in Sardinia could be traced to malaria outbreaks that once persisted on the island. In the 1930s, some 70,000 Sardinians were infected with malaria, according to the Rockefeller Foundation. By the 1950s, there were only three or four cases, thanks to a post-World War II effort (funded partly by the Rockefeller Foundation) to eradicate the disease-causing mosquitoes from the island.
When malaria was widespread, the infection-fighting B cells of people with the mutation would have produced a robust response, and those people would have survived the outbreaks, the researchers theorized. [27 Devastating Infectious Diseases]
"Malaria is a potent factor in evolution –– it kills children. So those people are never able to reproduce," David Schlessinger, a co-author of the study and chief oftheNational Institute on Aging's Laboratory of Genetics, told Live Science."If you don't get protection against malaria, you're gone. It's fiercely selective."
In Sardinia, the mutation made the population more resistant to malaria, but the trade-off was a higher incidence of autoimmune diseases, explained Mohamed Oukka, an immunologist at the University of Washington, and Seattle Children's Research Institute. Oukka was not involved in the new study, but wrote an editorial that was also published in the journal today about the new research.
"We have evolved through many plagues in human history by creating genetic mutations to fight off infections," Oukka told Live Science. "But then autoimmunity can become a problem."
This isn't the only case where increased vulnerability to one disease can make you better equipped to fight another. Researchers have long known that a small change in the gene for hemoglobin both causes sickle cell anemia and protects against malaria. And researchhas shown that herpes may offerincreased resistance against bacteria, including the bubonic plague.
The next step will be to try to use the Sardinia finding to develop drug therapies that could suppress the overstimulated B cells that contribute to multiple sclerosis and lupus. In fact, drugs that suppress the BAFF protein are already on the market, but different drugs target B-cell production through different pathways. [10 Deadly Diseases That Hopped Across Species]
However, such drugs may not work for all patients with multiple sclerosis and lupus, Oukka noted.
"People can have the same disease, but the underlying, driving force can vary from one person to another," Oukka told Live Science. "This is why some therapies work for some, but not others."
As for why so many people on the island manage to reach age 100, Oukka said he believes it has less to do with genetics and more to do with diet and lifestyle.
"They eat a lot of fish. They have less stress," he said. "That probably plays more of a role than anything."
Original article on Live Science.