Carbs Could Cause Trouble for Patients with Inflammatory Bowel Disease
CHICAGO — The nutrients in the food you eat can worsen or lessen symptoms of inflammatory bowel disease, a new study from Canada finds.
Inflammatory bowel disease involves having chronic inflammation in the digestive tract. The two main types of the condition are ulcerative colitis and Crohn's disease. An estimated 3 million adults in the U.S. have inflammatory bowel disease (IBD), according to a recent government survey, conducted by the Centers for Disease Control and Prevention.
Although the exact causes of IBD are not well-understood, "it makes sense that what you eat would have an effect on what's happening in your gut," said lead study author Dr. Christopher Sheasgreen, a fellow in inflammatory bowel diseases at the University of Toronto and Mount Sinai Hospital Toronto. Sheasgreen presented his findings here on May 6 at Digestive Disease Week, a scientific meeting focused on digestive diseases. [5 Ways Gut Bacteria Affect Your Health]
However, there's very little data available on how foods affect the gut, so Sheasgreen decided to investigate, he said.
In the new study, 69 IBD patients were asked to fill out food diaries three to four days before a scheduled colonoscopy. The patients had either Crohn's disease or ulcerative colitis, though some patients had not yet had their specific type of IBD determined.
Using specialized software, the researchers analyzed the food diaries for the amounts of various nutrients present in each person's diet. Then, the researchers looked at two outcomes: whether the patients were experiencing any symptoms (such as diarrhea or abdominal pain) and what was going on in their guts.
More than 60 percent of the patients had no symptoms of IBD, the researchers found.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
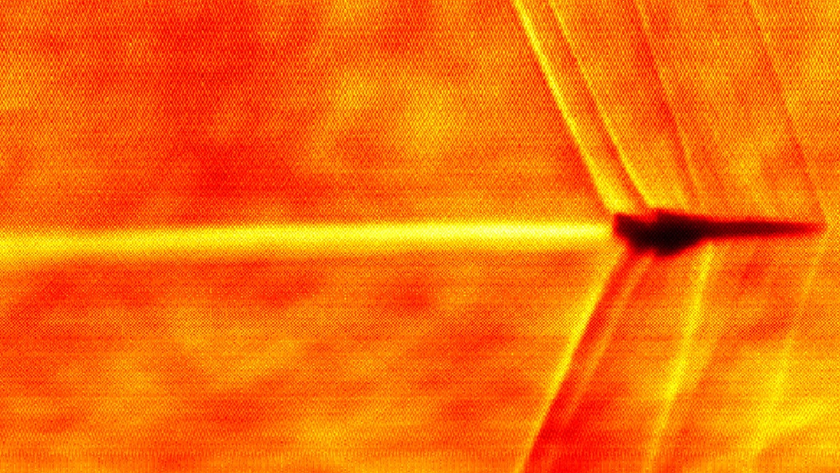
But the colonoscopies provided the researchers with information about what was happening on the inside of the patients' guts. The colon of someone during a flare-up of IBD looks different than the colon of someone who is not experiencing a flare-up, Sheasgreen told Live Science. Nearly 40 percent of the patients had no signs of flare-ups during their colonoscopies, the study said.
When the researchers compared these outcomes to the food diaries, the most interesting finding was that eating a greater amount of carbohydrates was associated with more symptoms of IBD, but no signs of an IBD flare-up in the gut, Sheasgreen said.
This finding seems "paradoxical," Sheasgreen said. However, one possible explanation is that the patient's symptoms could be linked specifically to types of carbohydrates called fermentable carbohydrates, he said. (The study didn't differentiate among types of carbs, he added.) These carbohydrates do cause abdominal symptoms, but they're not known to cause damage to the colon, he said. [The Poop on Pooping: 5 Misconceptions Explained]
A wide variety of foods contain these carbohydrates; that includes onions, apples, beans and certain artificial sweeteners.
The study showed only an association; it did not prove that carbohydrates cause these effects in people with IBD, Sheasgreen noted. More studies are needed to fully tease out the effects that different nutrients have on IBD, he said.
But the results can offer "a little bit of validation to patients" who say that the foods they eat affect their disease, he said.
Sheasgreen also noted that it's common for patients with IBD to have symptoms even when the individuals are not having a flare-up, just as people who don't have IBD also experience stomach pain and diarrhea from time to time.
The findings have not yet been published in a peer-reviewed journal.
Originally published on Live Science.