How Bad Is Gonorrhea's Resistance to Drugs? Some Cases Are Untreatable
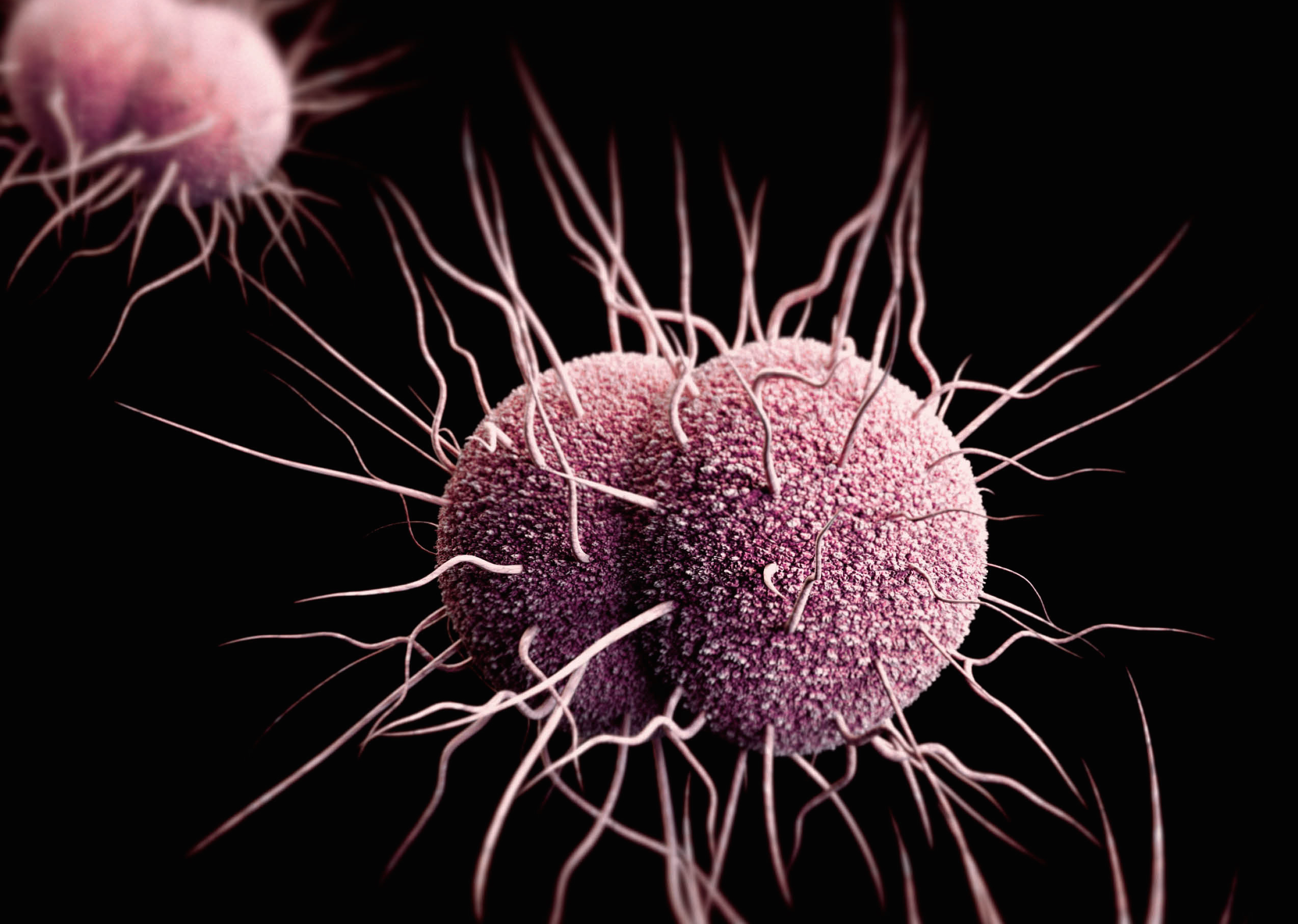
The sexually transmitted disease gonorrhea is becoming increasingly more difficult, or at times even impossible, to treat because strains of the bacteria that cause it have become resistant to antibiotics, according to a new report.
In the report, researchers looked at data from gonorrhea cases and antibiotic resistance from 77 countries. Of all countries that reported such data between 2009 and 2014, 97 percent reported cases of the disease that were resistant to the gonorrhea treatment ciprofloxacin, 81 percent reported cases that were resistant to another treatment called azithromycin, and 66 percent reported cases that were resistant to the treatment called cephalosporin, the researchers found.
"The bacteria that cause gonorrhea are particularly smart," Dr. Teodora Wi, medical officer of human reproduction at the World Health Organization (WHO), who co-authored the report, said in a statement. "Every time we use a new class of antibiotics to treat the infection, the bacteria evolve to resist them." [27 Devastating Infectious Diseases]
Some countries with good surveillance of the disease have reported cases of gonorrhea that were resistant to all known antibiotics, according to the report. "These cases may just be the tip of the iceberg, since systems to diagnose and report untreatable infections are lacking in lower-income countries where gonorrhea is actually more common," Wi said.
About 78 million new gonorrhea cases are diagnosed each year worldwide, the researchers said. Reports from many countries with good surveillance of the disease have suggested that gonorrhea has been on the rise, the researchers said. For example, the number of gonorrhea cases in the United Kingdom increased by 11 percent between 2014 and 2015, according to the report. The global increase in gonorrhea cases has been partially due to decreasing condom use, increased travel, low rates of gonorrhea-infection detection and inadequate treatment, the researchers said.
Complications from gonorrhea can be particularly dangerous for women, increasing their risk of developing pelvic inflammatory disease, infertility, HIV infection and ectopic pregnancy (where a fertilized egg grows outside the uterus), the researchers said.
Gonorrhea's resistance to antibiotics has been spreading the most in Asia, North America, Europe, Latin America, the Caribbean and Australia, according to the report.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Researchers are testing three new potential drugs for gonorrhea treatment: solithromycin, zoliflodacin and gepotidacin, the researchers said. Pharmaceutical companies may not be eager to invest in developing new gonorrhea treatments, because such treatments are taken for only short periods of time, which makes them less profitable than, say, treatments for chronic diseases. Moreover, the effectiveness of the drugs wanes as the bacteria develop resistance, which in turn feeds the need to constantly develop new drugs to treat gonorrhea, the researchers said.
Many people who contract gonorrhea show no symptoms, and so they do not get diagnosed or treated, the researchers said. [6 Superbugs to Watch Out For]
Another problem is that people may have symptoms such as a discharge from the urethra or the vagina, which can be due to other conditions besides gonorrhea. Doctors may assume this symptom is due to gonorrhea and prescribe antibiotics to treat it, but this only perpetuates the cycle of antibiotic misuse and antibiotic resistance, the researchers said.
"To control gonorrhea, we need new tools and systems for better prevention, treatment, earlier diagnosis, and more complete tracking and reporting of new infections, antibiotic use, resistance and treatment failures," Dr. Marc Sprenger, director of antimicrobial resistance at WHO, said in a statement. Some of these tools include new antibiotics, improved diagnostic tests and a vaccine to prevent the disease, he said.
Originally published on Live Science.
Flu: Facts about seasonal influenza and bird flu
What is hantavirus? The rare but deadly respiratory illness spread by rodents