How Does the New 'Gene-Altering' Therapy Fight Cancer?
A new type of cancer treatment that involves altering a person's genes — and could save children's lives — passed a major hurdle this week, when a U.S. Food and Drug Administration (FDA) panel recommended that the agency approve the therapy, The New York Times reported. But how does the treatment work?
The treatment is for an uncommon type of leukemia, called B-cell acute lymphoblastic leukemia, that affects mainly children and young adults, according to the Times. The success rate of the treatment that was seen in a recent clinical trial was "astonishing," said Lee Greenberger, chief scientific officer of the Leukemia and Lymphoma Society (LLS). Greenberger was not involved directly in the research of the new therapy, but the LLS has contributed significant funding toward the work.
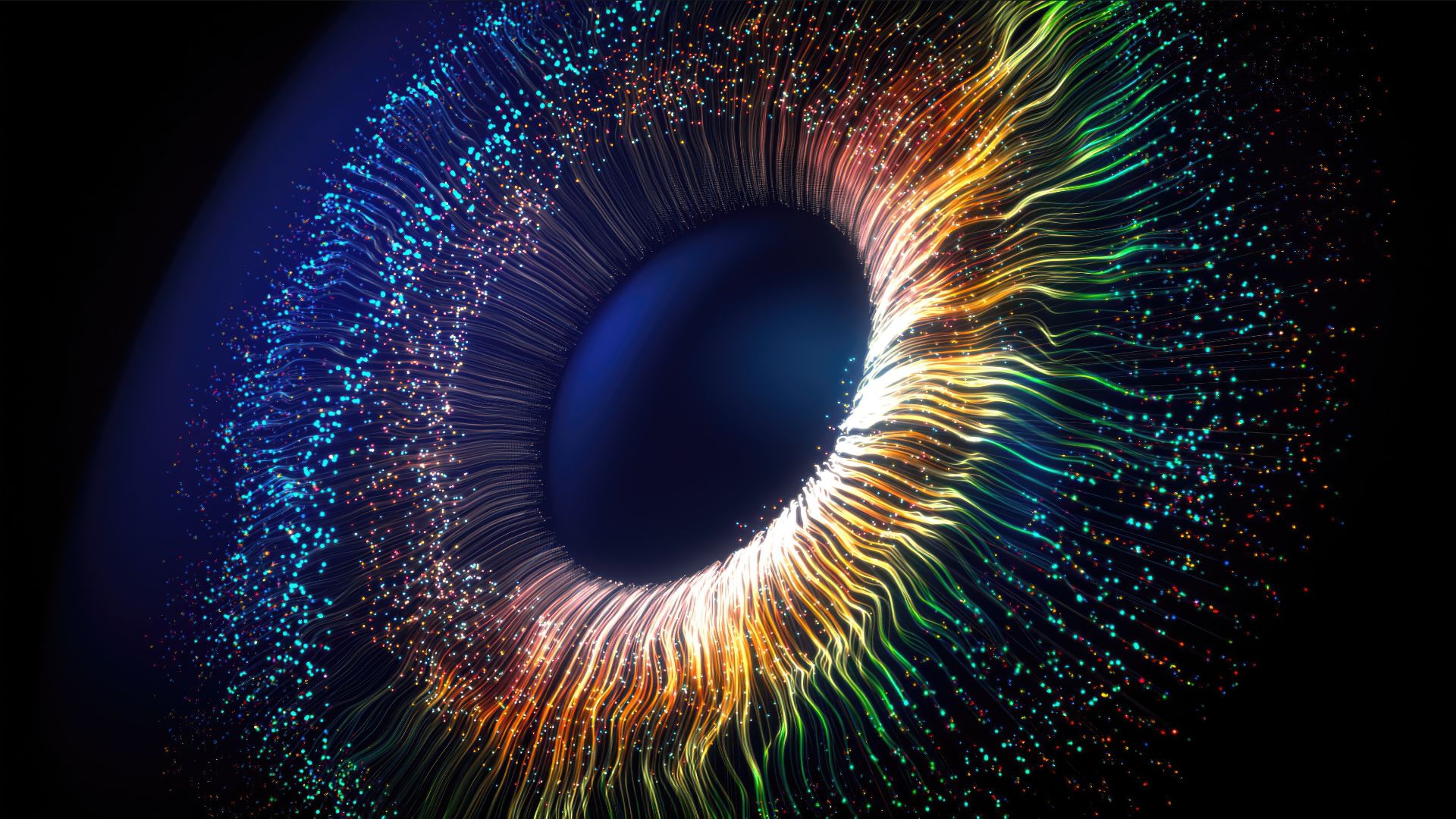
Leukemia is cancer of white blood cells, and it starts in the bone marrow, the soft material found in the center of bones that produces blood cells. [11 Surprising Facts About the Immune System]
Simply put, the new treatment works by rewiring a person's own immune cells to fight cancer.
To do this, doctors first remove millions of the immune cells, called T cells, from a patient's blood, Greenberger told Live Science. Normally, T cells help destroy infected or cancerous cells.
These T cells are sent to a lab to be purified, and then are genetically engineered, Greenberger said. Scientists mix the cells with a virus that works as a "vector" to insert a bit of genetic material into the cells' DNA. (Viruses commonly insert their DNA into living cells.) In this case, the vector that's used is an inactive form of HIV. After 15 to 25 days — during which the cells have started to produce the new protein that is encoded by the DNA, as well as grow and multiply — the "gene-altered" T cells are infused back into the patient.
"It's basically a one-time therapy," Greenberger said.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
The genetic material that the virus inserted into the T cells makes the cells do two things when they are put back into the patient's body, Greenberger said. First, the T cells produce an antibody that sits on the cell's surface, he said. This antibody enables the T cells to recognize the cancer cells. Also, the new genetic material activates the T cells so that, when they arrive at the tumor cells, they not only recognize them but also latch on and destroy them. [10 Do's and Don'ts to Reduce Your Risk of Cancer]
Once in the body, these "hunt and destroy" T cells multiply, so the patient ends up with an "army" of them in the blood, Greenberger said.
The entire process of the T cells killing the cancer cells lasts a couple of weeks, Greenberger said. But when the treatment is working, it can cause some serious side effects, he noted. The side effects include a condition called cytokine release syndrome, which can cause fevers, and another condition called neurotoxicity, which can cause symptoms such as disorientation and an inability to speak.
These side effects start as the T cells begin to kill the tumor cells, and when the tumor cells are depleted, the symptoms calm down, Greenberger said. During the entire process, however, the patient stays in the hospital and is monitored very carefully. In some cases, patients need intensive care.
In addition, some normal, noncancerous cells also carry the protein that the T cells are engineered to recognize. That means that the T cells will also kill these healthy B cells. "But people will survive without those [B cells]," Greenberger said. They do, however, need to get regular infusions of "immune globulins," which help to boost the immune system.
The FDA panel's recommendation was based on the results of a clinical trial run by the drug company Novartis, The New York Times reported. In the trial, 63 patients were given the new therapy, and 52 of them, or 83 percent, went into remission — meaning the cancer went away. The other 11 patients died.
Greenberger noted that the treatment is being recommended for leukemia patients who have no other options left. And based on the results of the research, "it works," he said. The FDA panel recommended that it be approved specifically for patients whose cancer has not responded to other treatments or whose cancer returned after treatment.
So far, the patients who were successfully treated with the new therapy sometime between April 2015 and August 2016 haven't had their cancer return and haven't developed any serious side effects, Greenberger said. Still, they'll need to be monitored over the long term to see if anything changes. Novartis plans on monitoring the patients for 15 years.
Originally published on Live Science.