Antibiotics, Agriculture & Superbugs: Q&A with 'Big Chicken' Author Maryn McKenna
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
In the United States alone, hundreds of thousands of poultry farms produced nearly 9 billion chickens for consumption in 2016, according to a report published in April by the U.S. Department of Agriculture (USDA). And all those chickens add up to big profits — a value of about $26 billion, the USDA reported. But the staggering popularity of chicken has come at an enormous cost — to chickens and to people.
The story of the demand for chicken is also a story of antibiotics, which spurred the growth of the chicken industry by literally fueling the growth of chickens, making broilers put on weight more quickly and with less feed. At the same time, greater numbers of chickens raised together in close quarters increased the risk of communicable diseases, encouraging the liberal use of preventative antibiotics to stave off the possibility of epidemics, according to science writer and journalist Maryn McKenna.
Over time, this contributed to an alarming rise in antibiotic-resistant bacteria, leading experts and officials to re-evaluate the way chickens were raised, and to formulate ways to counteract threats from drug-resistant superbugs. [Top 7 Germs in Food That Make You Sick]
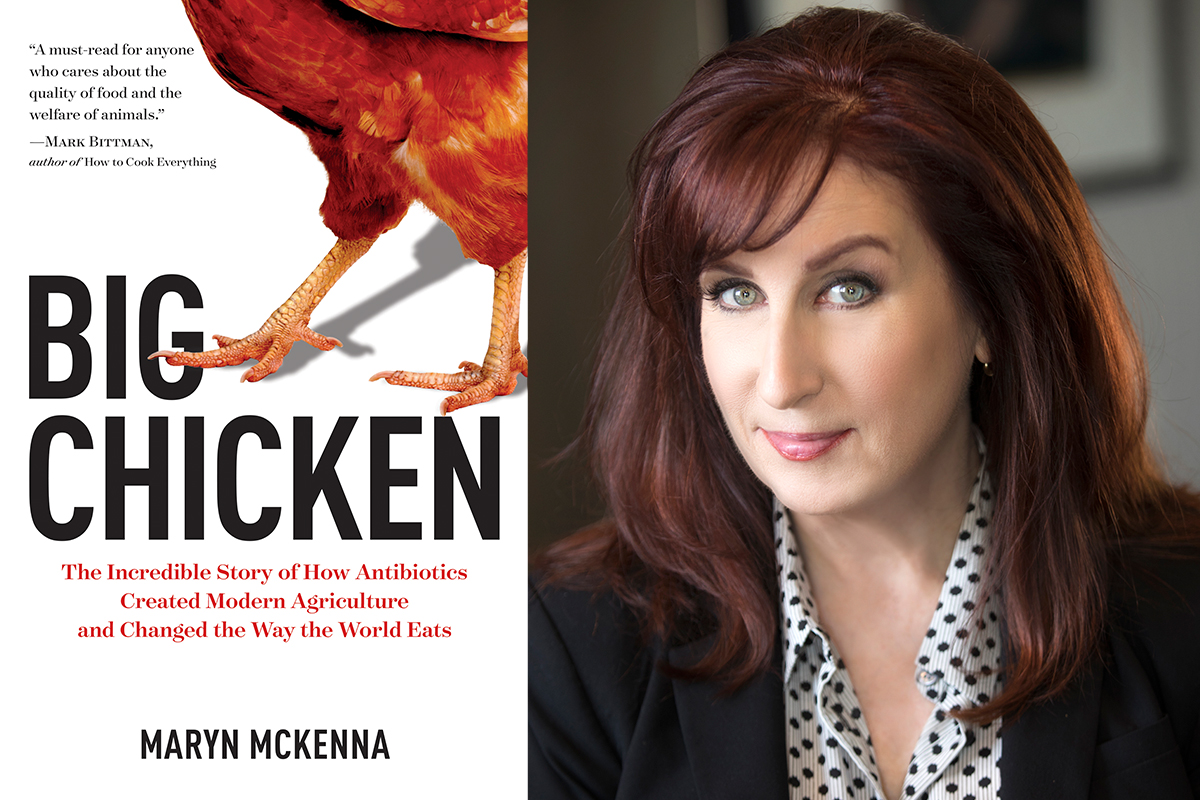
McKenna weaves together the intertwined story of industrial chicken farming and antibiotics in her new book, "Big Chicken: The Incredible Story of How Antibiotics Created Modern Agriculture and Changed the Way the World Eats" (National Geographic, 2017). McKenna recently spoke to Live Science about how chickens became such an overwhelmingly popular source of cheap protein; how the demand for chicken, in turn, transformed the use of antibiotics in livestock; and the repercussions that had for human health.
This Q&A has been edited lightly for length and clarity.
Live Science: What was it about chickens that led you down the path to writing this book?
Maryn McKenna: I was looking first at the issue of antibiotics in agriculture, which came from having written a book on antibiotic resistance ["Superbug: The Fatal Menace of MRSA" (Free Press, 2011)]. And in the process of that work, I came across this statistic: In the U.S., we sell four times as many antibiotics for use in animals as we do in people. Having just been listening to people be very emphatic in the medical realm that we have to use antibiotics conservatively, the fact that their caution and alarm could exist in the same time and space as literally tons of antibiotics [were] being given to animals — essentially with no oversight — was startling to me.
Get the world’s most fascinating discoveries delivered straight to your inbox.
As I dug more deeply into it, I realized that this story of antibiotic resistance and use in agriculture was bracketed by the story of how we raise chickens. Chickens were the first animals to get growth-promoter antibiotics experimentally, and chickens are probably going to be the first sector of the protein economy in the United States to exit routine antibiotic use. And it seemed to me that all the things we critique about poultry production — and, in fact, about industrial-scale livestock production — can all be traced back to the use of antibiotics.
Without antibiotics being used, we wouldn't have been able to produce animals so rapidly. We wouldn't have had the impetus to crowd them in barns and feed lots; antibiotics allowed them to be protected from diseases [that might have resulted] from that crowding. Antibiotics created a supply of reliable, inexpensive protein; then demand for it had to be stimulated by things like chicken nuggets and further processed chicken.
And so the more I looked, the more I realized that chickens really told the story of industrial-scale, modern, high-throughput livestock production better than anything else I could find.
Live Science: What were the red flags indicating that antibiotics used in chickens could have consequences for human health, and how did researchers connect the dots to convince policymakers that antibiotics promoting growth or being used for disease prevention in farm animals were making people sick?
McKenna:At the start of the story, nobody thinks that using antibiotics in animals is going to have any downside. To give them credit, the researchers in the late 1940s and early 1950s looked into what the use of antibiotics would do to the animals that were getting them, and concluded that if resistance occurred, then the growth promotion effect or the preventative effect would stop working — and they would know that it wasn't working because animals would cease gaining weight or they would start getting sick. They didn't think to look beyond the animal to see if there was going to be a human effect.
The very first signal that something was going wrong with antibiotics use in agriculture — which I love, because it's just so bizarre — is that in the early 1960s, people complained that children were developing penicillin allergies from drinking milk. And that turns out to be because so much penicillin is going into dairy cattle, that some milk in the U.S. and the U.K. could have been sold as a drug, because it had so much penicillin in it. Then, cheese makers start complaining that they can't make cheese anymore, because there's so much penicillin in the milk that when they put the culturing bacteria in, it kills them, and so the milk doesn't solidify into cheese.
There start to be epidemics of antibiotic-resistant foodborne illness— things like Salmonella and Campylobacter [bacteria] — and that's never been seen before. Big outbreaks that are not tied to a specific geographic area are new, and that they are antibiotic-resistant is very new.
And so a couple of epidemiologists in the U.K. and then in the U.S. do some really yeoman work, trying to track back illnesses from the sick people through the supply chain of what the people ate, back to the processors and then back to farms. That detective work takes a long time, but every time, they ended up back at a farm using antibiotics in its animals, and that happens over and over again.
In the late 1960s, it happened often enough that the British government empanels a commission to examine this issue of farm antibiotic use, and in 1969, they come out with a report that recommends the first-ever government action to stop this use of antibiotics [in all farm animals], which the U.K. does in 1971.
And then attention turns to the U.S., where there's a seminal experiment in 1976. Dr. Stuart Levy [a researcher at Tufts University specializing in antibiotics use and resistance] sets up an experimental farm on a family's property on the outskirts of Boston, and installs brand-new batches of chickens — widely segregated and unable to mix. He hires a member of the family, and she starts feeding antibiotic-laced feed to some of the chickens, and then watches to see if antibiotic-resistant bacteria are going to show up in those birds, in the other birds that have no contact with the first batch of birds, and in the farm family.
And in each case, that happens.
That's the first controlled demonstration that antibiotics given to farm animals produce antibiotic-resistant bacteria in the guts of the animals that receive them, that those bacteria can move through the environment and enter other animals and reproduce there, and that they can also contact humans.
On that basis, in 1977, the FDA tries to control antibiotics use in animals in the U.S. in the way that the U.K. did, and is prevented by political interference and enters this stalemate that persists until the Obama administration comes along. In that time, more and more, and larger and larger outbreaks happen, and the molecular tools for tracing them get more precise. By the time the Obama administration rolls around in 2010 and decides to change what could not be changed in 1977, the evidence is really incontrovertible that this has been causing negative human health effects.
Live Science: Have we reached a critical tipping point in the evolutionary arms race against drug-resistant bacteria, as some bacteria are already showing resistance to the "last resort" antibiotics in the human arsenal?
McKenna: We are at a point of significant peril, because bacteria are becoming so multiple-drug resistant, and are resistant to most serious "big gun" antibiotics that we have. And agriculture bears some responsibility for that. Not solely; it's important to say there is misuse and overuse of antibiotics in medicine as well. But if we were to stop using these antibiotics, there are indications we could send antibiotic resistance back down the evolutionary pathway.
There are societies that stopped using antibiotics in agriculture, and also slowed down their antibiotics use in medicine — Scandinavian countries and the Netherlands. When they took away the evolutionary pressure on bacteria to keep developing defenses, bacteria gave up some of those defenses, because they no longer needed them. Many mutations that protect bacteria against the action of particular antibiotics are costly to bacteria in an evolutionary sense; they make the bacteria otherwise less fit to survive in whatever niche they are occupying. If bacteria can give those up, they will. If antibiotics pressure goes away, then they no longer need that mutation.
In national surveys in Sweden, Norway, Denmark and the Netherlands, where they do excellent jobs of tracking occurrences of drug-resistant bacteria in humans and animals, you can see that after they gave up or prevented use of certain antibiotics, that the incidence of resistant bacteria is declining. It declines first in animals. And that's very clear; there's very robust evidence for that. And then it starts to decline in humans, too.
That doesn't work for everything. Some research not very long ago showed that bacteria in chickens in the U.S. were hanging on to resistance to a drug that is no longer used in chickens, the lone drug that was removed from the market a while ago. That's probably because it's a mutation that doesn't have any fitness cost [meaning it doesn't impact the animal's survival]. But generally speaking, if you take the antibiotics away, the resistance goes away. So that's one way that we could back ourselves away from the precipice.
Live Science: In recent years, the study of the human microbiome has revealed microbes to be critical players in our body systems. Has that helped to raise awareness in the chicken industry — and in the general public — about the dangers of antibiotics, which can kill helpful bacteria as well as harmful ones?
McKenna: Absolutely. I think that when all this started, we didn't even have the word "microbiome" to indicate what was going on, though it was pretty clear that growth promotion, at least, is a perturbation of the gut microbiome — that's what causes its effects to happen.
There's a widespread understanding now that we live in a microbial world, and everything we do to affect it has unintended consequences. I think that also contributes to this new caution about how freely we dispense antibiotics, because we understand we're setting forth unpredictable ripple effects that are going to perturb this entire microbial conversation in ways that we didn't really understand before.
You can buy "Big Chicken" on Amazon.
Original article on Live Science.

Mindy Weisberger is a science journalist and author of "Rise of the Zombie Bugs: The Surprising Science of Parasitic Mind-Control" (Hopkins Press). She formerly edited for Scholastic and was a channel editor and senior writer for Live Science. She has reported on general science, covering climate change, paleontology, biology and space. Mindy studied film at Columbia University; prior to LS, she produced, wrote and directed media for the American Museum of Natural History in NYC. Her videos about dinosaurs, astrophysics, biodiversity and evolution appear in museums and science centers worldwide, earning awards such as the CINE Golden Eagle and the Communicator Award of Excellence. Her writing has also appeared in Scientific American, The Washington Post, How It Works Magazine and CNN.
 Live Science Plus
Live Science Plus