Why You Might Need a Vaccine to Go to The Kentucky Derby

Kentucky Derby fans may need to take some extra precautions before heading off to the races.
The Indiana State Department of Health is recommending that its residents get vaccinated against hepatitis A and take other steps to protect themselves from the illness before traveling to Kentucky or Michigan, both of which are experiencing large outbreaks of the viral infection.
Kentucky has reported more than 300 cases of hepatitis A since November 2017, with 39 new cases reported in the first week of April, according to the Kentucky Department for Public Health. Most cases in the state have occurred around Louisville — the city where the Kentucky Derby is held. The famous horse race, which draws more than 150,000 people each year, takes place on the first Saturday in May.
"With popular tourist events coming up in other states, we know many Hoosiers will be traveling to areas impacted by hepatitis A, and we want them to be safe," Pam Pontones, the Indiana deputy state health commissioner, said in a statement. "Getting vaccinated and thoroughly washing your hands before and after preparing food and eating and after using the restroom are simple, safe and effective ways to prevent the spread of hepatitis A."
But do you really need to get a hepatitis A vaccine if you're going to the Kentucky Derby?
Dr. Amesh Adalja, a senior scholar at the Johns Hopkins Center for Health Security, said the Indiana recommendation is an interesting step to take, and it's not a bad idea. "I can see why they would advise it," Adalja said. "It's something that's an easy measure that can minimize risk." [27 Devastating Infectious Diseases]
At the same time, Adalja told Live Science that the risk of hepatitis A probably isn't very high for the average visitor to the Derby. A number of recent U.S. hepatitis A outbreaks, including the one in Kentucky, have occurred primarily among the homeless population and illicit-drug users — a group that may have limited access to clean toilets and handwashing facilities, which are important in preventing the spread of hepatitis A.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
But hepatitis A outbreaks can also occur through contaminated food, Adalja noted — for instance, if food workers contract the illness and handle food without properly washing their hands. (The Kentucky hepatitis A outbreak has not been linked with contaminated food, although it was recently reported that a McDonald's employee in Berea, Kentucky, south of Lexington, had the infection and could have potentially spread it to customers.) If Kentucky Derby-goers want to minimize their risk of getting the illness, "the vaccine is one way to do that," Adalja said.
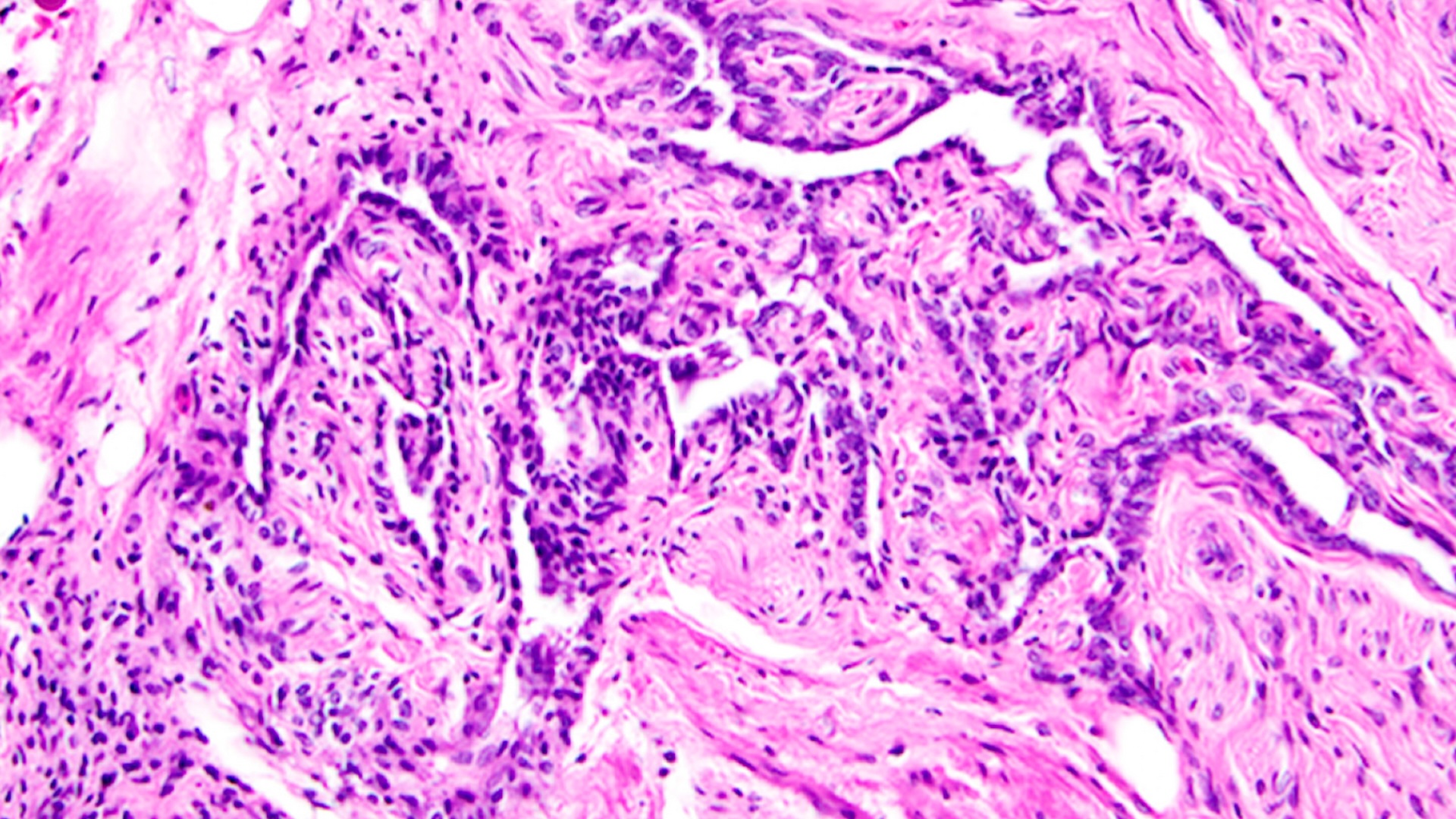
Hepatitis A is a contagious liver infection caused by the hepatitis A virus, according to the Centers for Disease Control and Prevention. The virus is spread through the "fecal-oral" route — that is, when small amounts of stool from an ill person contaminate objects, food or drinks that are then touched and ingested by another person, the CDC says. For this reason, thorough handwashing — particularly after using the bathroom or changing a child's diaper, or before eating — can help reduce a person's risk of getting hepatitis A, according to the Mayo Clinic.
It's important to note that the Indiana announcement is not a nationwide recommendation. In general, the CDC recommends the hepatitis vaccine for children at age 1, as well as adults who may be at higher risk for hepatitis A or for complications from the illness. These include travelers to countries where hepatitis A is common, people who use recreational drugs, people with chronic liver disease, men who have sexual contact with other men, and people who have direct contact with others who have hepatitis A.
The CDC says that ideally, a person should get the hepatitis vaccine two weeks or more before departing for their trip, but getting the vaccine any time before travel will provide some protection.
Adalja noted that a number of Americans are already vaccinated against hepatitis A. The vaccine was first licensed in 1995 and was recommended for all U.S. children starting in 2006. But that would still leave many adults today unvaccinated, unless they already got the vaccine for travel or because they fall into a group that's at higher risk for contracting the illness.
Symptoms of hepatitis A infection usually don't appear until two to six weeks after a person has been infected, and include fever, fatigue, nausea, vomiting, dark-yellow urine, joint pain and jaundice (a yellowing of the skin and eyes), according to the CDC.
People with the infection usually get better on their own without a specific treatment, but in some cases, the infection can lead to liver failure, particularly in older adults or people who have other liver diseases, according to the National Institutes of Health.
Original article on Live Science.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.