This Man Says a 'Rare Gene' Cured His Type 1 Diabetes. Experts Are Skeptical.

Type 1 diabetes, or diabetes mellitus, is an incurable disease that requires lifelong treatment. That is, unless you're Daniel Darkes.
About eight years ago, Darkes said, doctors diagnosed him with type 1 diabetes: a potentially life-threatening condition in which the immune system kills off the cells in the pancreas that produce insulin, the hormone necessary for transporting glucose, or sugar, into cells so they can produce energy.
But early last year, routine finger-prick tests showed his blood-sugar levels were normal, so doctors advised him to stop his insulin injections, Darkes said. Now, his doctors have told him they're 80 percent sure he's cured, the Northampton Chronicle and Echo reported. If true, this would mean Darkes could be the first person ever to naturally experience complete remission of type 1 diabetes. [27 Oddest Medical Cases]
Darkes has become a celebrity within the diabetes community, particularly in the United Kingdom, and he was happy to talk with Live Science about his experience.

But does Darkes' story really mean type 1 diabetes can be cured? Darkes declined to provide his medical records, and the experts Live Science spoke to said there were several missing or confusing pieces of information in his story. Usually, incredible medical stories like this one are reported as case reports in the medical literature, the experts said. And even if the details of his story can ultimately be confirmed, the experts emphasized that it's extremely unlikely that Darkes' case would lead to a widespread cure for type 1 diabetes, as reports in the media have wrongly suggested.
A lifelong diagnosis
Darkes, who is 30 years old and an army veteran, lives in Northamptonshire, England. Soon after he left the army, he began feeling symptoms of type 1 diabetes: sweating, blurred vision, tiredness and weight loss. "It lasted three or four days," Darkes told Live Science. "Then I collapsed at work."
Darkes said that a blood test showed his body wasn't producing C-peptide, a by-product of the body's production of insulin, which can reveal how much of the hormone the pancreas makes. Additional tests led doctors to diagnose him with type 1 diabetes, Darkes said.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
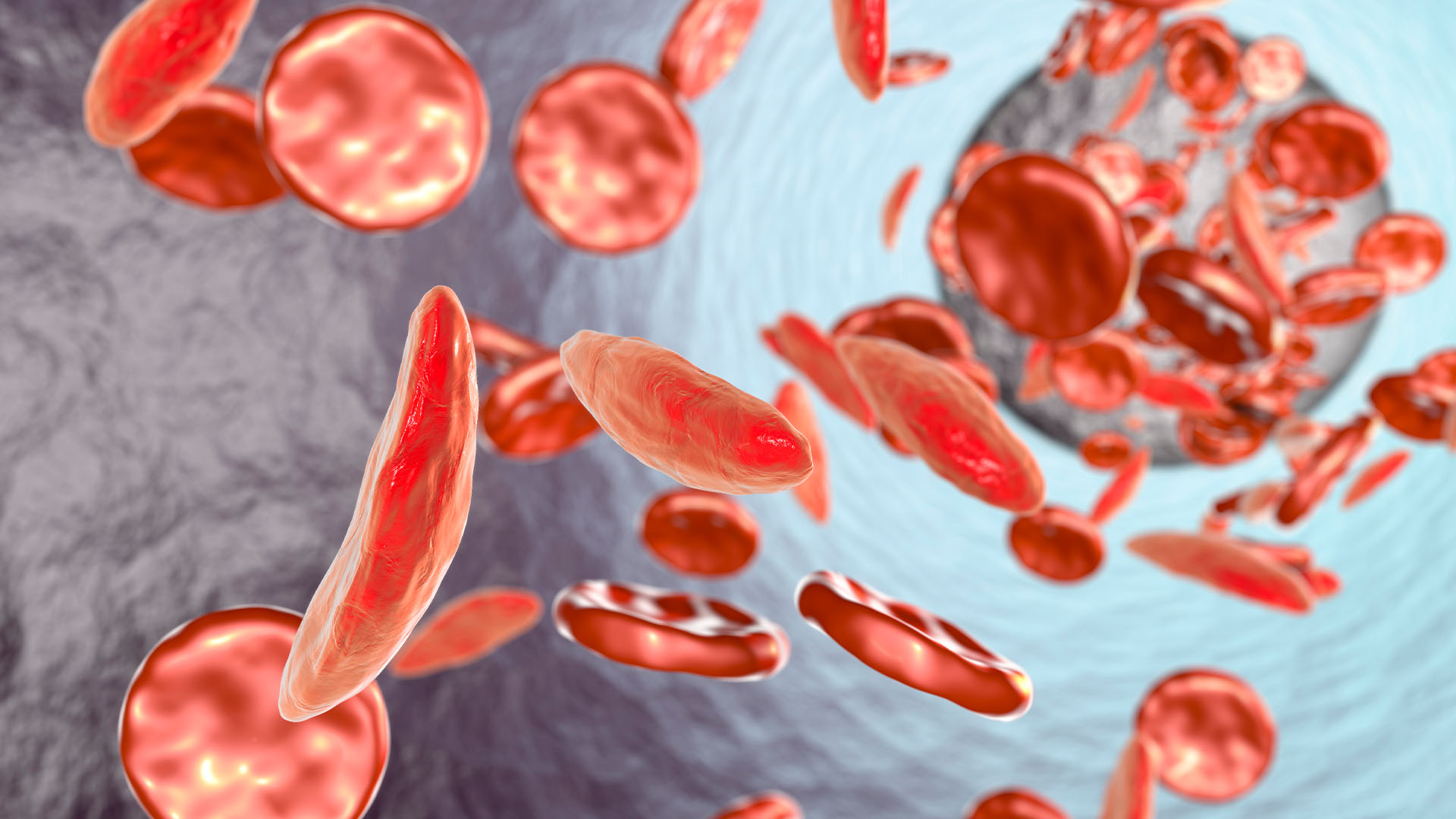
It's unclear how people get the disease — genetics plays a big role, though unknown environmental factors may also trigger the disease. Either way, the disease causes the immune system to mistakenly attack and kill insulin-producing cells, called beta cells, in the pancreas. (This differs from type 2 diabetes, in which the body initially makes sufficient insulin but the cells cannot properly use it.) Without enough insulin working to remove glucose from the blood stream, and allowing glucose to enter the body's cells, blood sugar levels spike. Left untreated, this insulin deficiency leads to a deadly complication called diabetic ketoacidosis. What's more, having high blood sugar over the long term can cause life-threatening complications such as kidney damage or heart disease, according to the Mayo Clinic.
The primary treatment for type 1 diabetes is lifelong insulin injections and consistent blood sugar monitoring. Darkes said he gave himself insulin injections four times a day to keep his blood sugar levels in check. But something changed in 2016, when he began training intensively for ultramarathons.
Darkes said his blood sugar began crashing, especially at night. Low blood sugar, or hypoglycemia, can cause fatigue, hunger and irritability and, if left untreated, can cause seizures or death.
"That lasted three or four weeks, so I decided to go to my doctor," Darkes said.
He visited Northamptonshire General Hospital, where he said doctors explained that he was experiencing hypoglycemia because his insulin injections were causing his body to remove too much glucose from his blood. Darkes said his doctors also told him that his test results suggested that his diabetes had disappeared.
Live Science requested Darkes' medical records from Northamptonshire General Hospital communications manager Eva Duffy. She said the European Union forbids the release of patient medical records or test results even with a signed waiver. Duffy would not confirm or deny any of Darkes' claims.
"His story surfaced a year and a half ago, and we have never commented on Daniel's situation at any point," Duffy told Live Science.

At the recommendation of his doctors at Northamptonshire General, Darkes said he traveled to St. Louis in January 2017, where he underwent additional testing. First, he said, "I had a microchip placed into my lower back where my kidneys sit to measure protein levels and blood sugar, where it stayed overnight."
But Dr. David Klonoff, a clinical professor of medicine at the University of California San Francisco's Diabetes Center, who specializes in biotechnology for diabetes, was perplexed by the microchip Darkes described.
"My job is to keep up with this stuff," Klonoff told Live Science. "When something's out there, there's a good chance that I've heard about it, but I haven't heard anything about this [technology]."
When he was in St. Louis, Darkes said, he also underwent a running test "aimed at me personally" (since the doctors knew he was an avid runner), and a blood test to measure key pancreatic molecules and "to see if cells were alive and what percentage," he said.
Darkes said several medical professionals worked with him when he was in St. Louis, but he could name only his senior consultant, Dr. Michael Berk. Berk is an endocrinologist who runs his own practice in St. Louis and is also a clinical associate at Washington University. Because Darkes declined a request to submit a medical release form to Berk's office, Live Science could not confirm key elements of his story, or whether or not he was even a patient of Dr. Berk.
The results of his medical tests are still being analyzed, Darkes said, but he hasn't needed insulin injections for a year and a half. "It took a long time to sink in," he noted. But Darkes is confident he no longer has type 1 diabetes. He said that doctors told him that he has a "rare" gene that somehow facilitated his cure. "I'm the only one who carries [the gene], at the moment," and there's no further explanation so far, he said.
Too good to be true?
The first media reports of Darkes' supposed cure, along with a similar description of the "rare" gene that partially explained it, began surfacing in February 2017. At the time, Darkes made it clear that his doctors in Northampton were still reviewing the test results, and that they would report on their findings soon. A story published in March 2017 in the Northampton Chronicle and Echo reported that Darkes' test results "are expected to be published next week."
But they haven't been published, and now well over a year has passed. So, what is going on?
"Yes, it's a frustrating case," Darkes told Live Science in an email. "But the doctors have to be as accurate as they can be with what's happened, so they've given a 2-year time scale for completed type 1 reversal." Darkes explained that if he can go without insulin injections for two years, his doctors will be 100 percent sure his diabetes is gone.
Darkes said he asked his doctors if he could share more information about his case with the media but was told "not to give details about the medical case and results at present," he said. "There's nothing I can do until my consultant and team finalize later this year."
This makes Darkes' story seem less plausible, said Dr. Matthias von Herrath, a professor of developmental immunology at La Jolla Institute in California, and an expert in type 1 diabetes. This type of claim is "earth-shattering," he said. "If it's not well corroborated, it's like your grandmother's rumor kitchen" — there's nothing backing the story. If there is a clinical record and the data are clear, the doctors should publish a case report, Von Herrath told Live Science.
"The rare-gene story makes me doubt whether this is truly type 1 diabetes," said Bart Roep, a clinical immunologist at City of Hope's Diabetes and Metabolism Research Institute in California. "About 5 to 11 percent of [type 1] diabetic patients are misdiagnosed. What they have is MODY," or maturity-onset diabetes of the young.
MODY is an inherited form of diabetes mellitus caused by a change in one of 11 genes, which results in the body not producing enough insulin, according to Harvard Medical School. MODY can look similar to type 1 diabetes, but its symptoms and treatment vary depending on which of the 11 genes is affected.
"There have been cases where patients were treated with insulin for years until they discovered it was a rare genetic variant" of MODY, Roep told Live Science. Those people are no longer diagnosed as having type 1 diabetes, and they may be able to manage their blood sugar levels with either oral drugs or diet and exercise changes, "but that would not be the same as being cured," Roep said.
What could be happening
Beta cells, the cells that produce insulin, can regenerate and regain function in some cases, Von Herrath said. There's a wide spectrum of severity when it comes to type 1 diabetes, and that means some people may lose virtually all of their beta cells while others may retain a portion of them.
"What is interesting is that some patients retain beta cell function for over 50 years," he said. "And, it seems if you retain some, that's a lot better." So, for Darkes to still have some functioning beta cells would not be impossible, but it wouldn't eliminate the disease, Von Herrath said. "Depending on how many beta cells he has, maybe his form of type 1 diabetes was not very severe."
"You only need 10 percent of your beta cells to supply sufficient insulin," Roep said. He said there have been a couple of rare cases where a patient had typical type 1 diabetes but could go through long periods without insulin injections. "Insulin needs can be a moving target, and if you have a lifestyle change it's very plausible that you have a lesser need for insulin, and you can deal with [diabetes] with the beta cells you have," Roep said.
Researchers have only recently started to realize that diabetes is a far more diverse disease than they used to believe, Roep said. And every unique case "shows us that we don't know what we think we know," he said. But because of that diversity, "we will never have a magic bullet, drug or pill that will cure everybody."
Von Herrath agreed, and said he's frustrated every time he sees an article or study claiming that a cure for diabetes is on the horizon. It's really not true, he said, and those kinds of statements give people false hope.
All of the experts who spoke with Live Science hope to see evidence of Darkes' story in the scientific literature soon, but they aren't holding their breath. "It's a very strange story," Von Herrath said. "At any rate, wish him good luck."
Original article on Live Science.

Kimberly has a bachelor's degree in marine biology from Texas A&M University, a master's degree in biology from Southeastern Louisiana University and a graduate certificate in science communication from the University of California, Santa Cruz. She is a former reference editor for Live Science and Space.com. Her work has appeared in Inside Science, News from Science, the San Jose Mercury and others. Her favorite stories include those about animals and obscurities. A Texas native, Kim now lives in a California redwood forest.