Learning Muscle Control Curbs Prostate Surgery Incontinence
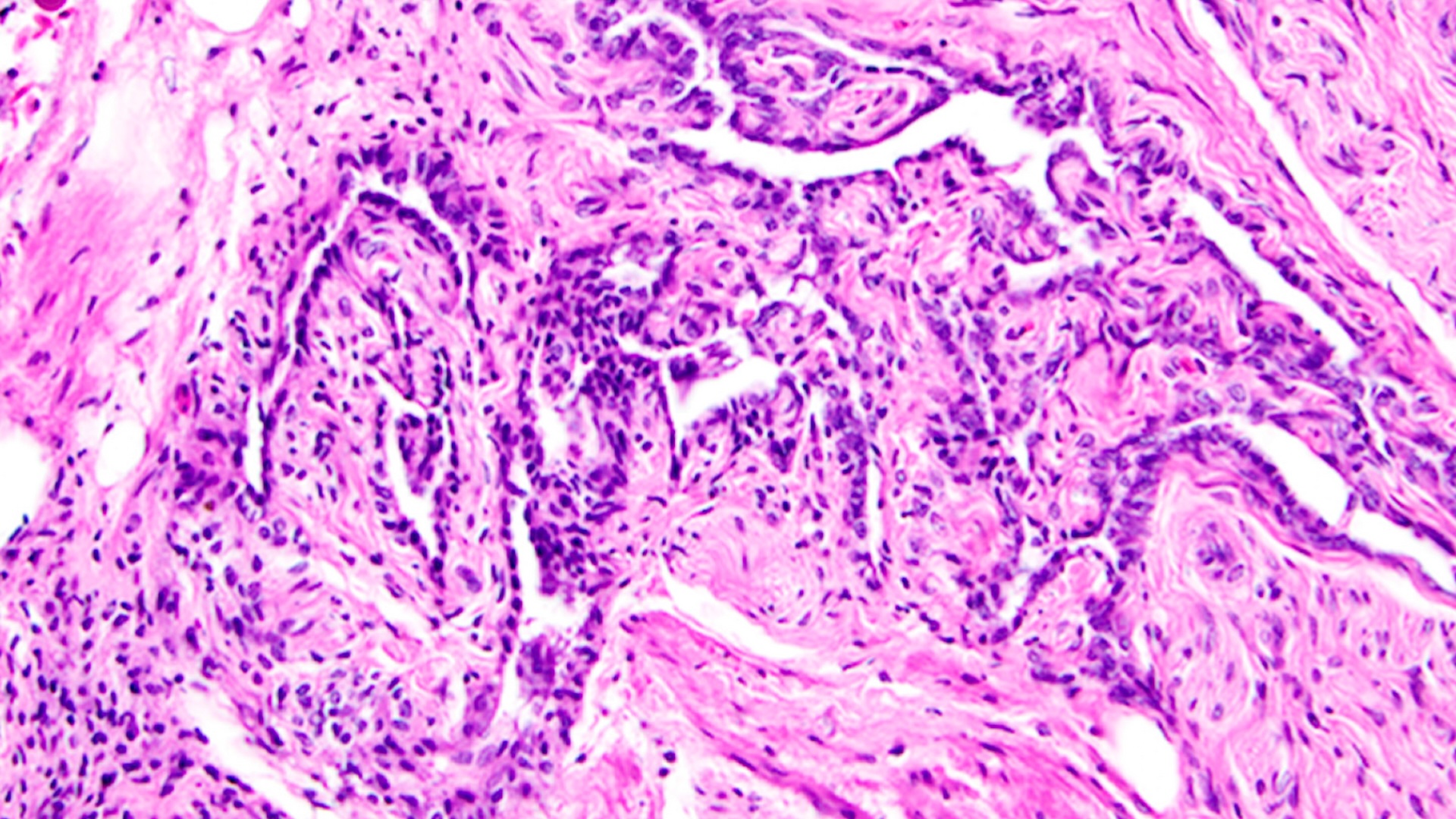
Teaching men techniques to control certain muscles can reduce urinary incontinence in those who have had their prostates surgically removed during cancer treatment, according to a new study.
The men in the study who used these techniques had a 55 percent reduction in incontinence episodes over eight weeks, compared with a 24 percent reduction in men who did not learn the techniques, the study said.
By learning how to contract their pelvic floor muscles, patients can strengthen them and control leakage, said study researcher Dr. Patricia S. Goode, professor of geriatric medicine at the University of Alabama at Birmingham.
Before the new study, there was only anecdotal evidence showing the effectiveness of using such "behavioral therapy" to treat patients who'd had this surgery, Goode told MyHealthNewsDaily. "Now that there is a randomized control trial, we are hoping more men will be able to undergo behavioral therapy."
Surgeons commonly treat prostate cancer patients with a radical prostatectomy, which removes the prostate gland. More than 140,000 U.S. men underwent the procedure between 1993 and 2003, according to a 2009 study in the journal BMC surgery.
But urinary incontinence is a common side effect of the surgery, and surveys show that as many as 65 percent of men have incontinence five years after surgery, the study said.
The study will be published tomorrow (Jan. 12) in the Journal of the American Medical Association.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Drops in incontinence
Goode and her colleagues tested ways to treat urinary incontinence in 203 men, ages 51 to 84, who had suffered from the condition for one to 17 years. All the men had previously undergone a radical prostatectomy.
The men were separated into three groups: one group underwent eight weeks of behavioral therapy, the second group had behavioral therapy along with biofeedback and electrical stimulation therapies, and the third group had no treatment for the eight weeks. (Biofeedback uses technology to amplify a bodily function, so a patient can monitor it, and electrical stimulation involves the use of an anal probe to promote the maximal contraction of pelvic floor muscles).
The researchers required the men to keep daily bladder diaries, and followed up with them one year after the treatments, the study said.
After eight weeks, the men who had undergone only the behavioral therapy saw a 55 percent drop in incontinence episodes — they went from having 28 to 13 episodes a week, on average. And 15.7 percent of them were able to completely control their urges, the study said.
The men who had the behavioral therapy along with biofeedback and electrical stimulation had 51 percent fewer episodes, dropping from 26 to 12 a week, on average. And 17 percent of these men could completely control their urges, according to the study.
These small differences suggested that adding biofeedback and electrical stimulation to behavioral therapies did not make a difference, Goode said.
The men who received no treatment had a 24 percent reduction in incontinence episodes, from 25 to 21 episodes a week, and 5.9 percent said they could completely control their urges, the study said.
A year later, the men who'd undergone behavioral therapy had 50 percent fewer incontinence episodes (13.5 a week), while the men with behavioral therapy plus the other therapies had 59 percent fewer episodes (9.1 episodes a week), according to the study.
Weighing the options
The study showed that behavioral therapy works to reduce incontinence, but many health care centers don't offer classes that teach men the techniques, Goode said.
Other treatments for incontinence include surgery and medications that affect neurotransmitter levels, but neither works for all men, Goode said.
"Surgery has risks, but the results are favorable," she said. However, "many men are reluctant to have another surgical procedure" after undergoing a radical prostatectomy.
Medications have side effects, and they can't be used for stress incontinence, the most common type men experience after prostatectomy, Goode said.
One example of a technique taught to the men is to "squeeze before you sneeze or cough or lift" to prevent stress incontinence, she said. Another is to stop and repeatedly squeeze the pelvic floor muscles instead of rushing to the bathroom.
"This will stop urgency, and then allow an unhurried trip to the bathroom with much less chance of leakage," Goode said.
Pass it on: Behavioral therapy can decrease incontinence episodes by 55 percent in men who have undergone a radical prostatectomy.
- 7 Cancers You Can Ward Off with Exercise
- 10 Dos and Don’ts to Reduce Your Risk of Cancer
- Prostate Cancer Patients Who Undergo Surgery Have High Survival Rates
Follow MyHealthNewsDaily staff writer Amanda Chan on Twitter @AmandaLChan.