Prior infection with common cold viruses won't protect against COVID-19

For months, scientists have wondered whether past exposure to seasonal coronaviruses that cause common colds might prevent people from getting a severe case of COVID-19.
TThat protection would explain why children, who get more of these colds, are less severely impacted by SARS-CoV-2, the coronavirus that causes COVID-19. But a new study, published Tuesday (Feb. 9) in the journal Cell, finds antibodies to such seasonable coronaviruses do not prevent SARS-CoV-2 infection or reduce disease severity.
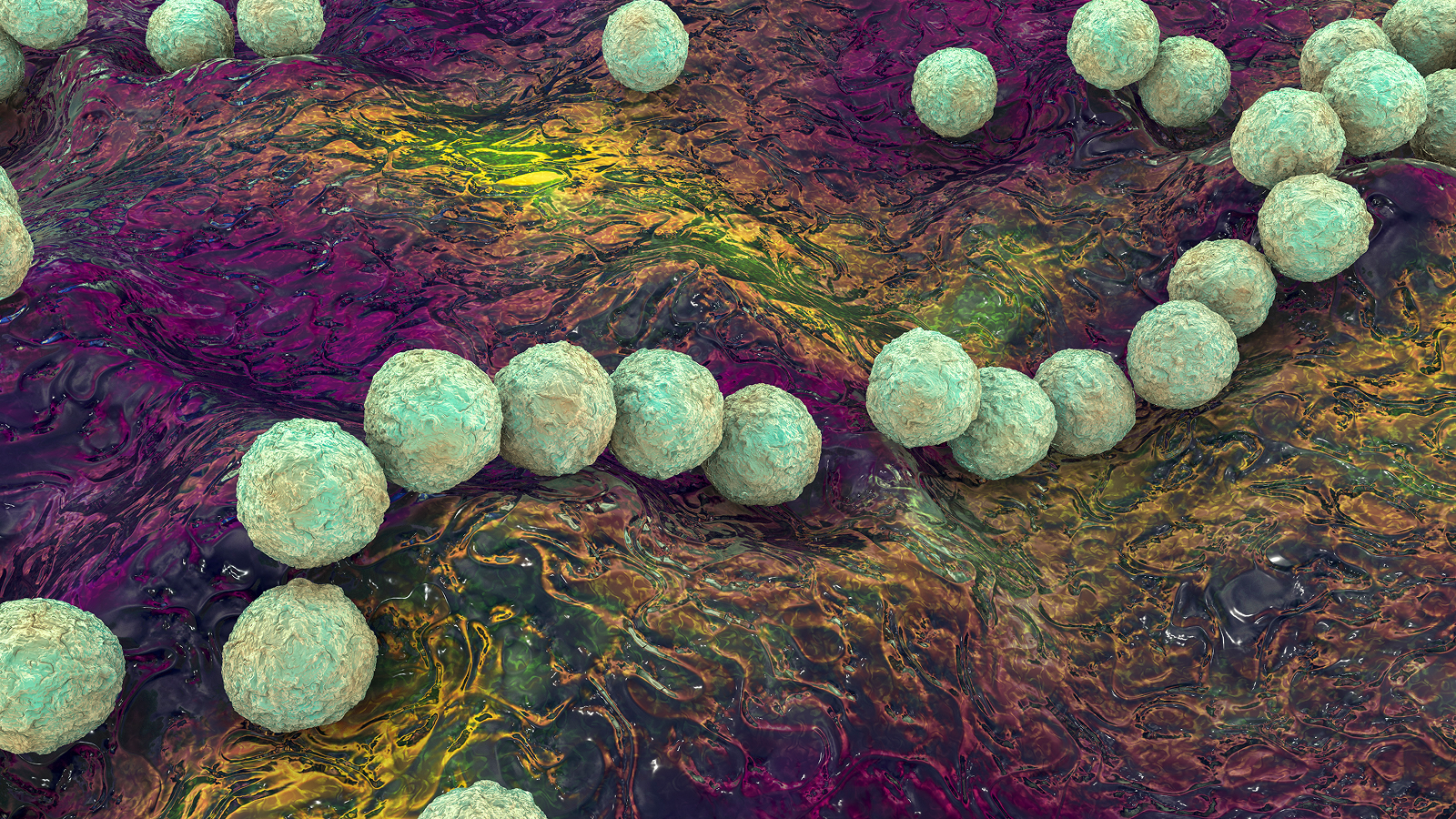
There are four coronaviruses that circulate in the human population and cause symptoms of a common cold — and most people have been exposed to them multiple times throughout their lifetimes (especially as children) and thus have developed antibodies against them. Researchers have conducted a number of studies in the past year to figure out if these antibodies could also bind to SARS-CoV-2 and protect against infection or severe disease.
Related: 20 of the worst epidemics and pandemics in history
"We found that many people possessed antibodies that could bind to SARS-CoV-2 before the pandemic, but these antibodies could not prevent infections,” senior author Scott Hensley, an associate professor of microbiology at the Perelman School of Medicine at the University of Pennsylvania, said in a statement. Nor could the antibodies stop severe disease.
This is a different conclusion from that of a similar study published in the journal Science in December, that found a small subset of people — and a higher proportion of children compared with adults — carried antibodies from previous coronavirus infections that had the ability to neutralize or disarm SARS-CoV-2.
It is "no surprise" that the new study found these antibodies can't prevent infection, said George Kassiotis, an immunologist at The Francis Crick Institute in the United Kingdom, who led the other study published in Science in December. Antibodies that work against multiple coronaviruses exist in only a few individuals and at very low levels, Kassiotis said. Children get sick with common colds much more than adults, which "means that their antibodies to common cold coronaviruses don’t even stop them [from] catching more common colds — it would be fairly odd if they could stop them catching the pandemic virus," he said.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
That's not the question, he said. Rather, researchers want to know if these antibodies can modify the disease once you've caught the virus, such as to protect you from severe symptoms, Kassiotis told Live Science. "The new study suggest[s] they don’t, but I don’t think this is conclusive."
Antibody archive
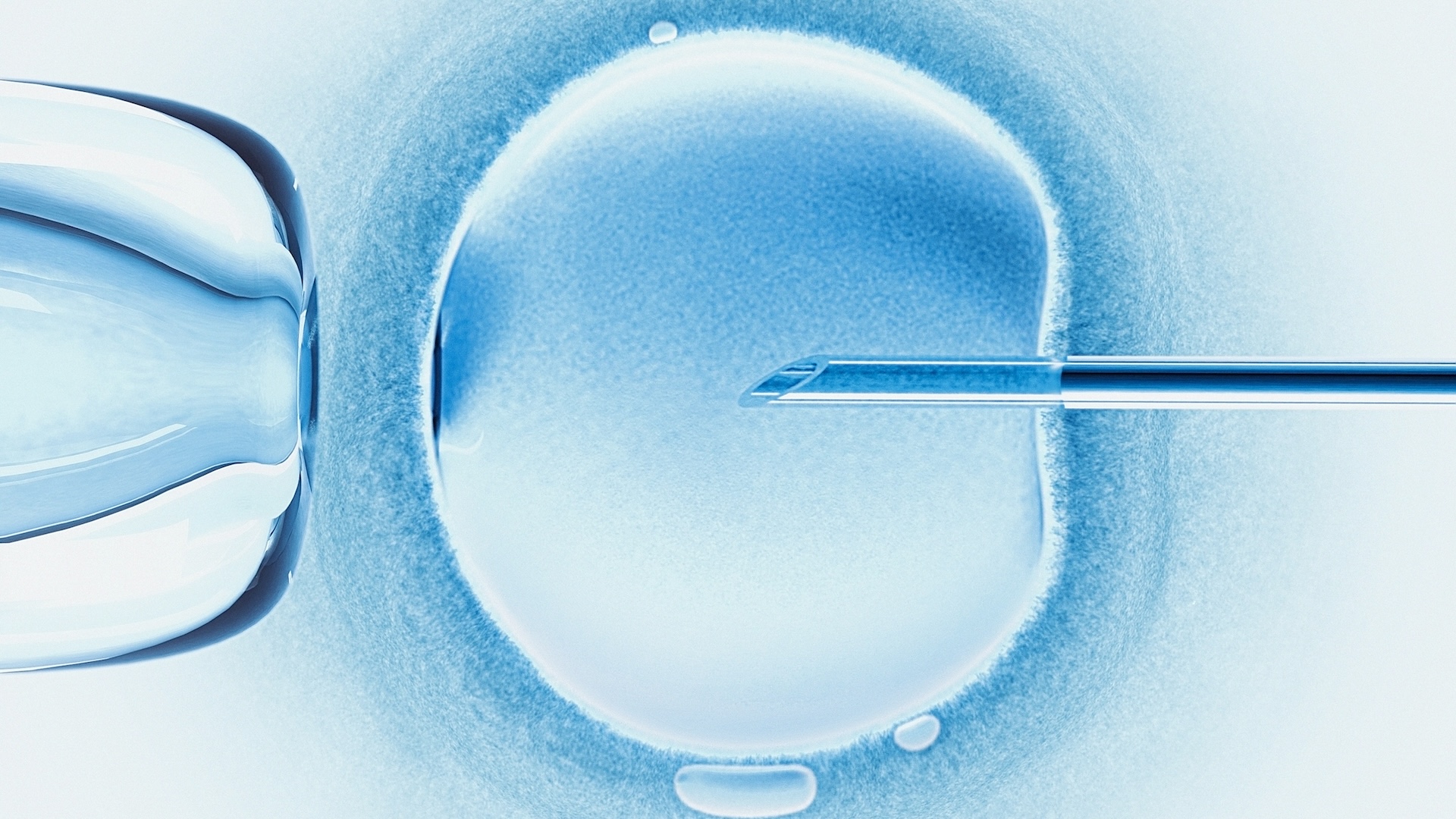
In the new study, Hensley and his team analyzed serum samples collected in 2017 to determine the level of antibodies against seasonal antibodies carried by the general population. Blood samples were taken from 263 children at the Children's Hospital of Philadelphia and from 168 adults at the Penn Medicine Biobank.
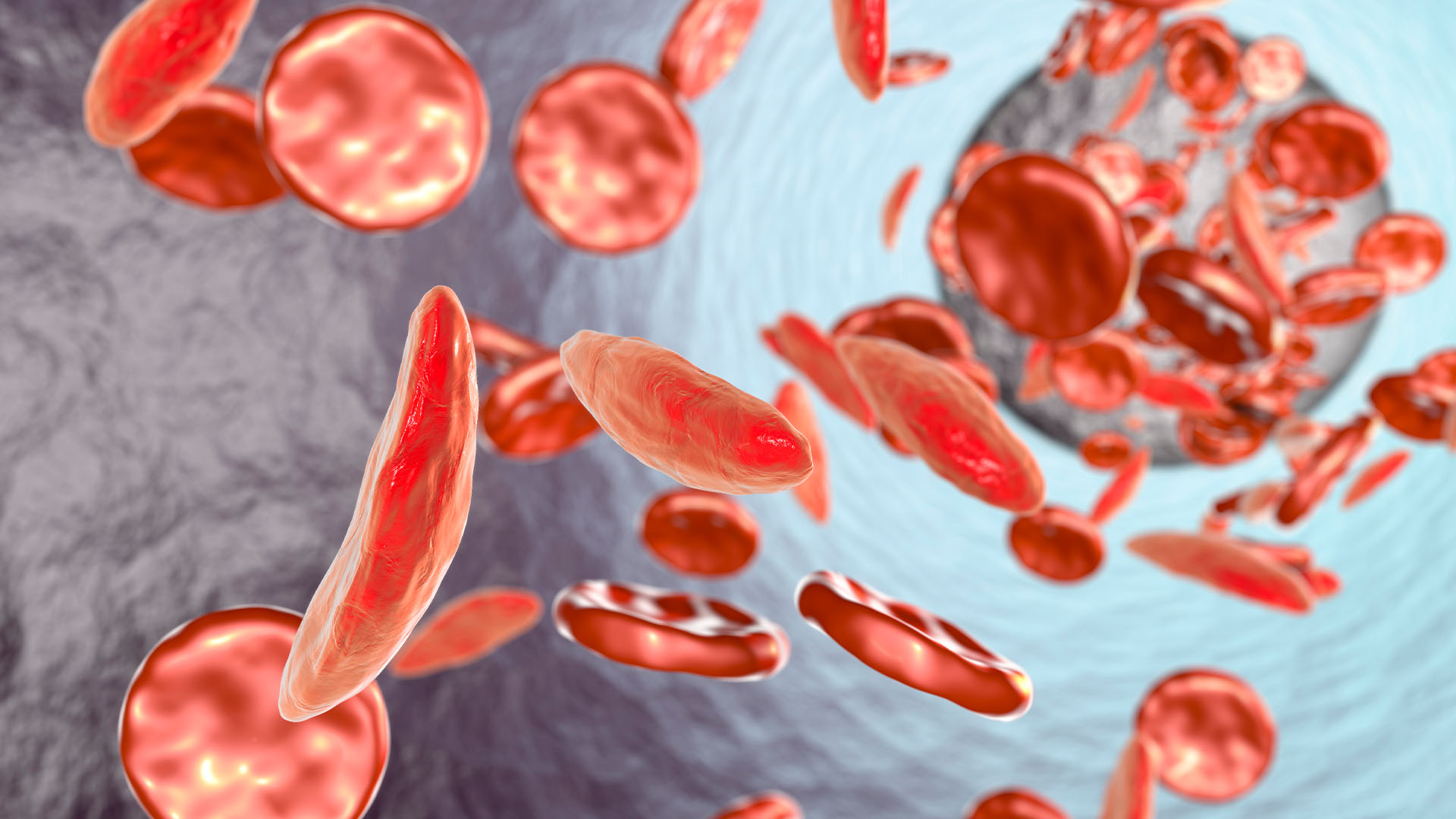
Most of these samples contained antibodies against seasonal coronaviruses, but only around 20% of them contained antibodies that also had the ability to bind to SARS-CoV-2's spike protein (the weapon the virus uses to invade human cells) or its nucleocapsid protein (a protein that's essential for the virus to replicate).
They then analyzed 502 other serum samples taken from people before the pandemic; half of these people tested positive for SARS-CoV-2 after the pandemic hit and half did not and were used as a control group. Similarly, they found that more than 20% of these samples contained coronavirus antibodies that could bind to SARS-CoV-2. However, people who had these antibodies still developed SARS-CoV-2. There was no correlation between the level of these antibodies and the severity of COVID-19 they developed, the study found.
In the third part of the experiment, they analyzed serum samples from 27 patients hospitalized with COVID-19 and found that the infection boosted the body's levels of antibodies against seasonal coronaviruses. Another study published in December 2020 in the journal Clinical Infectious Diseases similarly found that these antibodies didn't provide any neutralizing effects. But Kassiotis' study found that some of the antibodies that could bind to SARS-CoV-2 could neutralize the virus.
It's not clear if these discrepancies are due to differences in the way they tested their samples or other factors such as geographic differences, the authors wrote. Kassiotis thinks that it's because the researchers used a less sensitive test and so didn't identify enough people (two in the year before the pandemic and 11 total) with antibodies that could bind to the spike protein. "These numbers are far too small for any meaningful conclusion."
In any case, even if further, larger studies confirm that seasonal coronavirus antibodies are not protective, that doesn't mean there aren't other types of immune cells, other than antibodies that are lingering from past cold infections that could have a protective role and haven't yet been tested, according to the statement. For instance, T cells that respond to the original SARS-COV-1 virus stick around for decades, and some also bind to SARS-CoV-2, a July 2020 study in the journal Nature found.
"Although antibodies from prior coronavirus infections cannot prevent SARS-CoV-2 infections, it is possible that pre-existing memory B cells and T cells could potentially provide some level of protection or at least reduce the disease severity of COVID-19," Hensley said. "Studies need to be completed to test that hypothesis.”
Originally published on Live Science.

Yasemin is a staff writer at Live Science, covering health, neuroscience and biology. Her work has appeared in Scientific American, Science and the San Jose Mercury News. She has a bachelor's degree in biomedical engineering from the University of Connecticut and a graduate certificate in science communication from the University of California, Santa Cruz.